ELSEVIER
PRIMARY
TRANSITIONAL
CELL CARCINOMA
IN VESICAL DIVERTICULA
JACK BANIEL
AND
TALI
VISHNA
ABSTRACT
Objectives.
To evaluate
the treatment
and prognosis
of primary
tumors in bladder
diverticula.
Methods.
The cases of 61 1 patients
treated
for bladder
tumors at a single medical center were retrospectively reviewed.
Results.
Eight patients
had primary
intradiverticular
transitional
cell carcinoma.
Five patients
had Stage Ta
tumor, and 3 had Stage Tl tumor.
Most patients
were treated
by local resection
and adjuvant
intravesical
chemotherapy.
All patients
with initial Ta disease are disease free at the time of this writing.
One patient
with Tl disease died, 1 patient’s
disease
recurred
several times, and 1 patient
showed
positive
cytology
without
apparent
disease.
Conclusions.
Superficial
intradiverticular
tumors may be treated
conservatively.
Routine cystoscopy
for patients
with a bladder
diverticulum
is warranted
for early diagnosis
of possible
intradiverticular
tumor.
UROLOGY
50: 697-699,
1997. 0 1997, Elsevier Science Inc. All rights reserved.
eoplasms arising in a vesical diverticulum
are
of special interest because they present a complex disease treatment problem. The incidence of
neoplasms in vesical diverticula varies from 0.8%
to 10%.l12 The first report of a neoplasm occurring
in a diverticulum
was described in 1896.3 As in
other bladder tumors, diverticular neoplasms are
most prevalent in men above the age of 40 years.4
The relatively scarce documentation
of this disease
published in the literature suggests an overall poor
prognosis.2,5 It is postulated that the thin diverticular wall, which contains only a small amount of
smooth muscle (if any), facilitates early invasion.2
We review our experience in the treatment of 8
patients with neoplasms occurring within bladder
diverticula.
N
MATERIAL
AND
METHODS
Six hundred
eleven
cases of superficial
bladder
cancer
treated
between
1978 and 1995 were retrospectively
reviewed.
All patients
were followed
up at the outpatient
clinic at Rabin
Medical
Center,
Beilinson
campus,
Petach
Tikva,
Israel.
Of
these patients,
9 men also had a vesical
diverticulum,
and in
From the Department
of Urology,
Rabin Medical
Center (Beilinson campus),
Petach Tikva,
Israel
Reprint
requests:
Jack Buniel, M.D.,
Urology
Section, Rabin
Medical
Center,
Beilinson
Campus,
Petach Tikvu 49100, Israel
Submitted:
February
18, 1997, accepted
(with revisions):
May
13,1997
0 1997,
ELSEVIER SCIENCE
ALL RIGHTS RFSFRVFII
8 patients,
the primary
neoplasm
occurred
in a diverticulum.
The clinical
course,
diagnosis,
treatment,
and prognosis
were
also reviewed.
The patient’s
ages ranged
from 45 to 80 years,
with an average
age of 68.6 years. Follow-up
ranged
from 7
months
to 17 years, with a median
of 5 years.
RESULTS
The presenting symptom of all but 1 patient was
gross hematuria. The remaining patient presented
with dysuria. Intravenous
urography
(IVU) was
performed in 6 of the patients before surgery and
did not reveal any filling defect in the bladder.
Cystoscopy was performed in all 8 patients. In 7
patients, a tumor was seen inside a diverticulum.
In 1 patient, a second cystoscopy was diagnostic
and revealed a tumor.
The pathologic diagnosis in all patients was transitional cell carcinoma (TCC). Four patients had
poorly differentiated
carcinomas (grade III), 2 had
grade II carcinomas, and the remaining
2 had
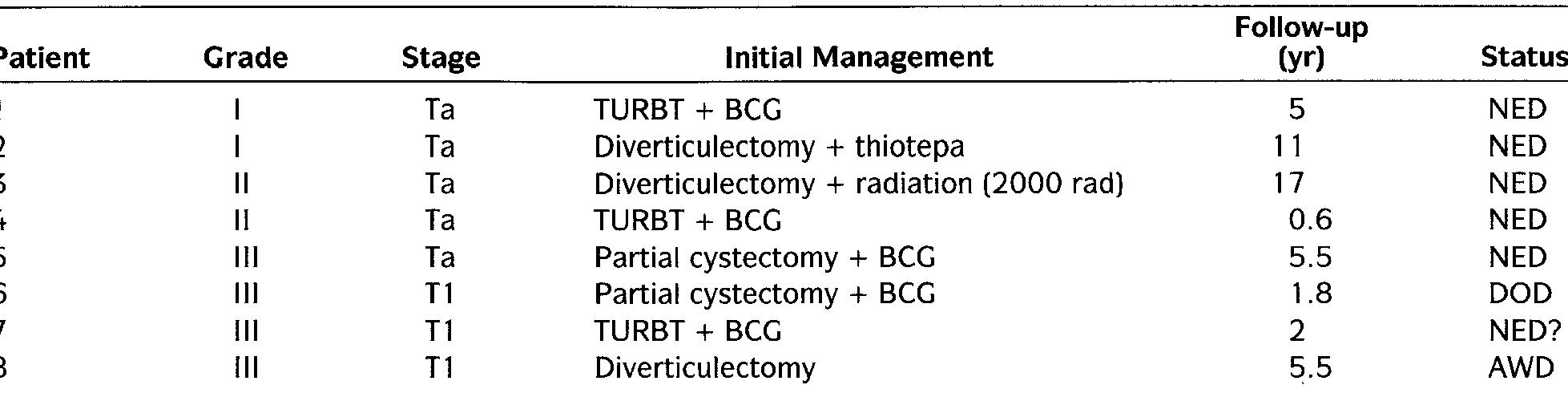
grade I carcinomas. Five patients had Stage Ta tumor and 3 patients had Stage Tl tumor (Table I).
Treatment is outlined in Table I. Open diverticulectomy was performed on 5 patients, and transurethral resection of the bladder tumor (TURBT)
was performed on 3 patients. Of the 5 patients who
underwent
diverticulectomy,
2 were treated postoperatively with bacille Calmette-GuCrin
(BCG)
instillations,
1 with thiotepa instillations,
1 with
postoperative
irradiation,
and 1 was followed up
INC.
0090-4295/97/$17.00
PII
soogo-4295(97)oo319-1
697
�TABLE
Patient
1
2
3
4
5
6
7
8
Grade
I.
Stage
I
I
II
II
III
III
III
III
Ta
Ta
Ta
Ta
Ta
Tl
Tl
Tl
KEY: AWD = alive with disease; KG
tumor.
= bacille Calmette-GuCrin;
Patient
management
Initial
Follow-up
M-1
Management
TURBT + BCG
Diverticulectomy
+ thiotepa
Diverticulectomy
+ radiation
TURBT + BCG
Partial cystectomy + BCG
Partial cystectomy + BCG
TURBT + BCC
Diverticulectomy
(2000 rad)
COMMENT
Vesical tumors occurring in diverticula pose a
difficult treatment problem because of their generally poor prognosis.4,6-8 This poor prognosis is
mainly a result of difficulty in diagnosis and early
invasion. It is difficult to diagnose a tumor in a
diverticulum.7
In our study, IVU was not diagnostically successful in 6 patients. Even cystoscopy
failed to reveal the existence of a tumor in 1 of the
8 patients.
The second and more important reason for poor
prognosis is believed to result from the anatomy
of the diverticulum.
Bladder diverticula are pseu-
Status
NED
NED
NED
NED
NED
DOD
NED?
AWD
5
11
17
0.6
5.5
1.8
2
5.5
DOD = dead of disease; NED = no evidence of disease; TLJRBT = transurethral
without
postoperative
treatment.
All 3 patients
who underwent
TURBT received adjuvant intravesical BCG instillations.
The survival data are
outlined in Table I. Four patients are disease-free
5 or more years beyond diagnosis. One patient is
disease free after 7 months of follow-up, and 1 patient has died. All patients with Stage Ta disease
are alive. Three patients had TlG3 disease. One
patient died of disease. He was treated by diverticulectomy and postoperative
BCG intravesical instillation. Sixteen months after initial diagnosis, he
had occurrence of pulmonary metastasis and died.
Another patient with TlG3 disease was managed
by TURBT and BCG instillations.
He was diseasefree for 2 years, and at the time of this writing has
no positive cytology with no apparent disease. Another patient with initial TlG3 disease is under
follow-up for 5.5 years; he had several recurrences,
the first occurring 4 years after initial diagnosis.
His disease recurred in a ureter and nephroureterectomy was performed.
Histology
revealed a
poorly differentiated
tumor with muscular involvement. Currently he is receiving adjuvant chemotherapy.
Five patients were staged as Ta. Four
patients have follow-up of more than 5 years and
are disease-free. One patient who was recently
treated is without
evidence of disease for 7
months.
698
and follow-up
resection of the bladder
dodiverticula;
they appear in areas deficient in
muscle fibers and are composed of mucosa and
serosa alone. The lack of muscle fibers in a diverticulum may allow the tumor to invade earlier and
more easily than in a normal thick muscle containing bladder wall. 2,9-11This also raises the question of accurate staging. Because muscle is absent
or deficient, should invasion of the lamina propria
(Tl) be synonymous in this case with Stage T2/T3
disease in normal bladder? In this study, only 3 of
8 patients (37.5%) had a potentially
invasive tumor, and were defined as having Stage Tl disease.
In other studies, the majority of patients presented
with high stage tumor. Faysal and Freiha6 found
nine (69.2%) invasive and only four (30.8%) noninvasive tumors arising in a diverticule. Lowe et
a1.7 described 5 cases of tumors in diverticula, all
of which were invasive. At present, lack of sufficient data on this topic precludes the creation of a
special staging system for diverticular tumors. The
tendency is to treat Tl tumors more aggressively.
Garzotto et al.” presented a highly aggressive
management plan in which 8 patients were treated
by diverticulectomy
and a combination
of chemotherapy and radiotherapy.
Their study did not
specify initial stage and cannot be compared to the
above. Because cancer of the bladder occurs predominantly
in men, most of the patients with tumor in a diverticulum
are men2,4,6,10,11 who are
over the age of 40 years.6”o In this study, all patients were men, and the average age was 68.6
years. The histology of the cancer in this study, as
in many others, was transitional
cell carcinoma.6,7,10
The survival rate of patients in this study, unlike
other reports, is relatively high (2-year survival
rate of 87.5%; S-year survival rate of 71.4%). Lowe
et a1.7 described 6 cases of tumors in diverticula.
Only 1 of the 6 patients survived after 2 years.
Faysel and Freiha6 described 12 cases of tumors
within a diverticulum
with results better than
Lowe’s (2-year survival rate of 58.3%), but no paUROLOGY
50 (51, 1997
�tients survived after 5 years (9 of 9 had died); tumor recurrence was reported in 91.7% of the patients. Montague and Boltuch”
described a fair
prognosis but with limited follow-up; 90% of their
patients survived after 2 years. In Montague’s
study, management
of patients did not differ
markedly from other series, and only 1 of 10 patients had had a total cystectomy. These authors
claim that the low mortality rate was due to early
detection. In their study, 40% of the patients were
diagnosed with Stage Ta disease. In this study,
62.5% of the tumors were noninvasive, which may
be the reason for the low mortality rate observed.
Even where aggressive management was implemented, as in the study by Garzotto et u1.,12 survival was 50%, with a median of 3.2 years. It may
be assumed that for Ta tumors, conservative treatment may suffice.
Early detection of tumors may result from better
imaging studies or from more frequent cystoscopies. In our study, 6 patients had IVU, and none
were diagnosed with tumor. Cystoscopy, on the
other hand, failed to detect the tumor only once.
Cystoscopy is very important in the detection of
tumors in diverticula.’ Some studies6a12,13 claimed
that aggressive treatment improves the prognosis
of patients with carcinoma in a diverticulum.
In
this study, even though most of the patients were
treated conservatively, the outcome was fair.
The incidence of neoplasms in bladders with a
diverticulum
is higher than the incidence of neoplasms within a normal bladder, ranging from
0.8% to lOoA When there is a diverticulum
and
neoplasm in the same bladder, most of the neoplasms will be located within the diverticulum.2,14
In our study, we found 9 patients who had both a
bladder tumor and a diverticulum.
Only in 1 patient did the tumor appear outside of the diverticulum.
The coexistence of neoplasms and diverticula
can be explained by stagnation of urine within the
diverticulum,
allowing local carcinogens to act on
the walls of the diverticulum.
Urine promotes
chronic irritation and inflammation,
and all factors
together act as promoters of carcinogenesis.2,4z9 Diverticula increase the risk of neoplasm of the bladder, and a neoplasm inside a diverticulum
has a
poor prognosis unless diagnosed early; thus, we
recommend
routine cystoscopy for any patient
who appears to have a diverticulum.*~1° Patients
UROLOGY
50 is), M7
with outflow obstruction are prone to develop vesical diverticula and thus comprise a group at risk
for the occurrence of an intradiverticular
lesion.
Intravenous urography or other radiographic studies may not be sufficient for timely detection of
diverticular tumors.
When dealing with invasive bladder diverticular
tumors (Tl), disease management should probably be aggressive (radical cystectomy versus diverticulectomy
plus adjuvant intravesical treatment), although the paucity of cases precludes
clear recommendation
of cystectomy versus local
resection.4’12’14 We conclude that early detection is
the key to improving the overall survival rate of
patients presenting with this disease, and that the
punishment
should fit the crime-the
treatment
should be aggressive only if the tumor is invasive.
REFERENCES
1. Lawrence WW (Ed): Current Surgical Diagnosis and
Treatment, 10th ed. Englewood Cliffs, New Jersey, PrenticeHall, 1994, pp 952-954.
2. Melekos MD, Asbach HW, and Barbalias GA: Vesical
diverticula: etiology, diagnosis, tumorgenesis and treatment.
Analysis of 74 cases. Urology 30: 453-457,
1987.
3. Targett JH: Diverticula of the bladder, associated with
vesical growths. Trans Path Sot London 47: 155, 1896.
4. Ostroff EB, Alperstein JB, and Young JD Jr: Neoplasm
in vesical diverticule: report of 4 patients, including a 21 year
old. J Urol 110: 65-69, 1973.
5. Micic S, and Ilic V: Incidence of neoplasms in vesical
diverticule. J Urol 129: 734-735, 1983.
6. Faysel MH, and Freiha FS: Primary neoplasm in vesical
diverticule: a report of 12 cases. BrJ Urol53: 141-143, 1981.
7. Lowe FC, Goldman SM, and Oesterling JE: Computed
tomography in evaluation of transitional cell carcinoma in
bladder diverticule. Urology 34: 390-395, 1989.
8. Johansen TE: Primary neoplasms in vesical diverticule.
Report of two cases. Stand J Urol Nephro122: 347-348,1988.
9. Kelalis PP, and McLean P: The treatment of diverticulum of the bladder. J Urol 98: 349-352, 1967.
10. Montague DK, and Boltuch RL: Primary neoplasms in
vesical diverticulae: report of 10 cases. J Urol 116: 41-42,
1976.
11. Das S, and Amar AD: Vesical diverticulum
associated
with bladder carcinoma: therapeutic implications. J Urol 136:
1013-1014,
1986.
12. Garzotto MG, Tewati A, and Wajsman Z: Multimodal
therapy for neoplasms arising from a vesical diverticulum. J
Surg Oncol62: 46-48, 1996.
13. Abeshouse BS, and Goldstein AE: Primary carcinoma
in a diverticulum
of the bladder; a report of four cases and a
review of the literature. J Urol 49: 534, 1943.
14. Knappenberger
ST, Usan AC, and Meilcow MM: Primary neoplasms occurring in vesical diverticulae. A report of
18 cases. J Urol 83: 153, 1960.
699
�
 Jack Baniel
Jack Baniel