Perineal nerve
| Perineal nerve | |
|---|---|
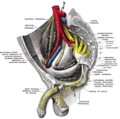
 Pudendal nerve, its course through the lesser sciatic foramen, and branches, including inferior anal at bottom right. | |
 The superficial branches of the internal pudendal artery. (Perineal nerve visible but not labeled.) | |
| Details | |
| From | Pudendal nerve |
| Innervates | Perineum, scrotum or labia majora, superficial transverse perineal muscle, bulbospongiosus muscle, ischiocavernosus muscle, bulb of penis, levator ani, external anal sphincter |
| Identifiers | |
| Latin | nervi perineales |
| TA98 | A14.2.07.039 |
| TA2 | 6556 |
| FMA | 21866 |
| Anatomical terms of neuroanatomy | |
The perineal nerve is a nerve of the pelvis. It arises from the pudendal nerve in the pudendal canal. It gives superficial branches to the skin, and a deep branch to muscles. It supplies the skin and muscles of the perineum. Its latency is tested with electrodes.
Structure
[edit]The perineal nerve is a branch of the pudendal nerve.[1][2] It lies below the internal pudendal artery. It accompanies the perineal artery. It passes through the pudendal canal for around 2 or 3 cm.[1][2] Whilst still in the canal, it divides into superficial branches and a deep branch.[1] The superficial branches of the perineal nerve become the posterior scrotal nerves in men,[3] and the posterior labial nerves in women.[1] The deep branch of the perineal nerve (also known as the "muscular" branch) travels to the muscles of the perineum.[1] Both of these are superficial to the dorsal nerve of the penis or the dorsal nerve of the clitoris.[4]
Function
[edit]The perineal nerve supplies the skin and muscles of the perineum.[1] The superficial branches supply sensation to the perineum, and the scrotum in men or the labia majora in women.[1] The deep branch supplies superficial transverse perineal muscle, the bulbospongiosus muscle, the ischiocavernosus muscle, the bulb of penis, levator ani, and the external anal sphincter.[1]
Clinical significance
[edit]The latency of the perineal nerve can be measured with electrodes.[5] It is used to test nerve function.[5]
Additional images
[edit]-
Sacral plexus of the right side. (Perineal nerve visible at center right.)
References
[edit]![]() This article incorporates text in the public domain from page 968 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 968 of the 20th edition of Gray's Anatomy (1918)
- ^ a b c d e f g h Rea, Paul (2015). "3 - Lower Limb Nerve Supply". Essential Clinically Applied Anatomy of the Peripheral Nervous System in the Limbs. Academic Press. pp. 101–177. doi:10.1016/B978-0-12-803062-2.00003-6. ISBN 978-0-12-803062-2.
- ^ a b Vaida, George T.; Jain, Sudheer K. (2010). "6 - Anesthetic Complications in Urologic Surgery". Complications of Urologic Surgery - Prevention and Management. Saunders. pp. 57–82. doi:10.1016/B978-1-4160-4572-4.X0001-5. ISBN 978-1-4160-4572-4.
- ^ Essential Clinical Anatomy. K.L. Moore & A.M. Agur. Lippincott, 2 ed. 2002. Page 263
- ^ de Groat, William C.; Yoshimura, Naoki (2015). "5 - Anatomy and physiology of the lower urinary tract". Handbook of Clinical Neurology. Vol. 130. Elsevier. pp. 61–108. doi:10.1016/B978-0-444-63247-0.00005-5. ISBN 978-0-444-63247-0. ISSN 0072-9752. PMID 26003239.
- ^ a b Swash, Michael (2008). "33 - Sphincter Disorders and the Nervous System". Neurology and General Medicine (4th ed.). Churchill Livingstone. pp. 633–650. doi:10.1016/B978-044306707-5.50036-5. ISBN 978-0-443-06707-5.
External links
[edit]- Anatomy photo:41:10-0100 at the SUNY Downstate Medical Center - "The Female Perineum: The Perineal Nerve"
- Anatomy image:9174 at the SUNY Downstate Medical Center
- Anatomy image:9187 at the SUNY Downstate Medical Center
- figures/chapter_32/32-3.HTM: Basic Human Anatomy at Dartmouth Medical School