Isotretinoin
 |
|
 |
|
| Systematic (IUPAC) name | |
|---|---|
|
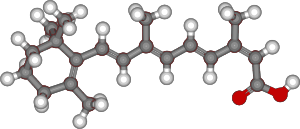
(2Z,4E,6E,8E)-3,7-dimethyl-9-(2,6,6-trimethylcyclohex-1-en-1-yl)nona-2,4,6,8-tetraenoic acid
|
|
| Clinical data | |
| Trade names | Accutane |
| AHFS/Drugs.com | monograph |
| MedlinePlus | a681043 |
| Licence data | US FDA:link |
| Pregnancy category |
|
| Legal status | |
| Routes of administration |
Oral, topical |
| Pharmacokinetic data | |
| Bioavailability | Variable |
| Protein binding | 99.9% |
| Metabolism | Hepatic |
| Biological half-life | 10–20 hours |
| Excretion | Renal and fecal |
| Identifiers | |
| CAS Number | 4759-48-2 |
| ATC code | D10AD04 (WHO) |
| PubChem | CID: 5282379 |
| IUPHAR/BPS | 7600 |
| DrugBank | DB00982 |
| ChemSpider | 4445539 |
| UNII | EH28UP18IF |
| KEGG | D00348 |
| ChEBI | CHEBI:6067 |
| ChEMBL | CHEMBL547 |
| Chemical data | |
| Formula | C20H28O2 |
| Molecular mass | 300.44 g/mol |
|
|
|
|
| (verify) | |
Isotretinoin (INN) (etymology and pronunciation), also known as 13-cis retinoic acid and first marketed as Accutane by Hoffmann-La Roche, is an oral pharmaceutical drug primarily used to treat severe nodular acne. Rarely, it is also used to prevent certain skin cancers (squamous-cell carcinoma), and in the treatment of other cancers. It is used to treat harlequin-type ichthyosis, a usually lethal skin disease, and lamellar ichthyosis. It is a retinoid, meaning it is related to vitamin A, and is found in small quantities naturally in the body. Its isomer, tretinoin, is also an acne drug.
Isotretinoin is primarily used as a treatment for severe acne. The most common adverse effects are a transient worsening of acne (lasting 2–3 weeks), dry lips (cheilitis), dry and fragile skin, and an increased susceptibility to sunburn. Uncommon and rare side effects include muscle aches and pains (myalgias), and headaches. Isotretinoin is known to cause birth defects due to in utero exposure because of the molecule's close resemblance to retinoic acid, a natural vitamin A derivative which controls normal embryonic development.
In the United States a special procedure is required to obtain the pharmaceutical. In most other countries a consent form is required which explains these risks. Women taking isotretinoin must not get pregnant during, and for 1 month after isotretinoin therapy. Sexual abstinence, or effective contraception is mandatory during this period. Barrier methods by themselves (such as condoms) are not considered adequate due to the unacceptable failure rates of approximately 3%. Women who fall pregnant whilst on isotretinoin therapy are generally counselled to have a termination. Isotretinoin has no effect on male reproduction.[1]
In 2009, Roche decided to remove Accutane from the US market after juries had awarded millions of dollars in damages to former Accutane users over inflammatory bowel disease claims. Other common brands are Roaccutane (Hoffman-La Roche, known as Accutane in the United States before July 2009),[D 1] Amnesteem (Mylan),[D 2] Claravis (Teva),[D 3] Absorica (Ranbaxy),[D 4] Isotroin (Cipla), and Epuris (Cipher).[2]
Contents
Medical uses
Isotretinoin is used primarily for severe cystic acne and acne that has not responded to other treatments.[3][4] Acne treatment usually begins with topical retinoids (e.g., tretinoin, adapalene), in combination with topical antibiotics (e.g., clindamycin, erythromycin) or antiseptics (e.g., benzoyl peroxide-containing preparations), followed by oral antibiotics (e.g., doxycycline or minocycline). In women a cyproterone acetate-containing contraceptive pill can be useful if there are no contraindications.
In cases of hormonal acne, such as in women in their 20s and 30s with cyclical acne, often a course of isotretinoin can permanently improve acne obviating the need for lifelong hormonal manipulation.[medical citation needed]
Indications
The primary indication for Isotretinoin is the treatment of severe cystic acne vulgaris.[5][6] Many dermatologists also support its use for treatment of lesser degrees of acne that prove resistant to other treatments, or that produce physical or psychological scarring.[7]
It is also somewhat effective for hidradenitis suppurativa and some cases of severe acne rosacea.[6] It can also be used to help treat harlequin ichthyosis, lamellar ichthyosis and is used in xeroderma pigmentosum cases to relieve keratoses. Isotretinoin has been used to treat the extremely rare condition fibrodysplasia ossificans progressiva. It is also used for treatment of neuroblastoma, a form of nerve cancer.
Isotretinoin therapy has furthermore proven effective against genital warts in experimental use, but is rarely used for this indication as there are more effective treatments. Isotretinoin may represent an efficacious and safe alternative systemic form of therapy for RCA of the cervix. In most countries this therapy is currently unapproved and only used if other therapies failed.[8][9]
Prescribing restrictions
Isotretinoin is a teratogen; there is about a 20%–35% risk for congenital defects in infants exposed to the drug in utero, and about 30%–60% of children exposed to isotretinoin prenatally have been reported to show neurocognitive impairment.[10] Because of this, there are strict controls on prescribing isotretinoin to women who may become pregnant and women who become pregnant while taking isotretinoin are strongly advised to terminate their pregnancies.[10]
In most countries, isotretinoin can only be prescribed by dermatologists or specialist physicians; some countries also allow limited prescription by general practitioners and family doctors. In the United Kingdom[11] and Australia,[12][13] isotretinoin may be prescribed only by or under the supervision of a consultant dermatologist. Because severe cystic acne has the potential to cause permanent scarring over a short period, restrictions on its more immediate availability have proved contentious.[14] In New Zealand, isotretinoin can be prescribed by any doctor but subsidised only when prescribed by a vocationally-registered general practitioner, dermatologist or nurse practitioner.[15]
In the United States, dispensing of isotretinoin is by an FDA-mandated website called iPLEDGE. iPLEDGE has applied to isotretinoin prescriptions since 1 March 2006. Under it, dermatologists must register their patients on the system before prescribing isotretinoin. Pharmacists must then verify the prescription on the iPLEDGE website before dispensing isotretinoin. The website allows no more than thirty days' supply of the drug to be prescribed or dispensed; and after issuance, another prescription may not be written for at least 30 days (even in the case of lost prescriptions). Prescriptions expire from iPLEDGE if not picked up from the pharmacy seven days after issuance. Physicians and pharmacists must verify written prescriptions on the system before filling an isotretinoin prescription. Due to the teratogenic effects of isotretinoin, iPLEDGE makes additional requirements of female patients filling prescriptions for the drug: women with child-bearing potential must commit to using two forms of effective contraception simultaneously for the duration of isotretinoin therapy and for a month immediately preceding and a month immediately following therapy.[16] Alerts continue to exist against purchasing isotretinoin online.[17]
Most other national health services emphasise that isotretinoin is a teratogen, but do not impose the same stringent conditions on the dispensing process as the United States does. In Mexico and Brazil the use of the drug is restricted: official identification and a signature must be provided by the patient before an isotretinoin prescription will be filled by a pharmacist.
Clinical guidelines for most countries recommends or mandates that the dispensing physician monitor patients, or provide instructions to the patient's regular doctor for monitoring. As part of the monitoring, patients' blood is periodically re-tested throughout treatment for blood lipids, pregnancy, and several other factors. Women, diabetics, and patients with liver problems are particularly at risk and will be monitored especially closely.
Dosage
The dose of isotretinoin patients receive is dependent on their weight and the severity of the condition. High-dose treatments are administered between 0.5 mg/kg/day to 2 mg/kg/day (usually at 0.5 to 1 mg/kg/day,[18] given as a single dose with food). Usually a course will last 8–10 months. A second course may be required. Efficacy appears to be related to the cumulative dose of isotretinoin taken, with a total cumulative dose over each course of 120–150 mg/kg used as a guideline.[5][6]
Nearly all patients achieve initial clearing of acne during a normal course of isotretinoin therapy. 90% of patients achieve excellent clearance of their acne after a cumulative dose of 150 mg/kg.
Lower-dosage treatments, such as 10–20 mg/day (approximately half the high dosage treatments above), can also be effective, with greatly diminished side effects.[19][20][21][22][23][24][25] However, such lower dosage courses may be associated with higher relapse rates, requiring additional courses, especially if not taken for sufficient time.[26][27][28][29][30]
Usually, a starting dose of 20 mg is taken with the largest meal of the day. After a few months, the dose is increased, e.g., to 40 mg/d. If side-effects permit, a higher dose such as 60 mg/d can be prescribed although daily dose rarely exceeds 60 mg. If 20 mg capsules are supplied, patients may take (for example) 20 mg one day, then 40 mg the next to provide an average daily dose of 30 mg/d. In most cases, isotretinoin achieves a complete clearing of acne during a standard-dose 12–16 week course. Some patients' acne will respond to a course before recurring, necessitating multiple courses of treatment.[31]
Adverse effects
Increasingly higher dosages will result in higher toxicity, resembling vitamin A toxicity. The following are adverse drug reactions from Roche's UK product information for Roaccutane as of October 2010:[32]
|
Type of disorders |
Very common (≥ 1/10) |
Common (≥ 1/100, < 1/10) |
Rare (≥ 1/10 000,< 1/1000) |
Very rare (≤ 1/10 000) |
|---|---|---|---|---|
| Infections |
bacterial infection |
|||
| Blood and lymphatic system |
|
|
||
| Immune system |
|
|||
| Metabolism | ||||
| Psychiatric |
|
|
||
| Nervous system |
|
|||
| Eye |
|
|
||
| Ear |
|
|||
| Vascular |
allergic vasculitis) |
|||
| Respiratory, thoracic and |
|
with asthma) |
||
| Gastrointestinal |
|
|||
| Hepatobiliary |
|
|||
| Skin and |
|
|
||
| Musculo-skeletal and |
|
and tendons)
|
||
| Kidney and urinary | ||||
| General |
|
|||
| Investigation |
|
|
|
Possible permanent effects
An Accutane medication guide approved by the U.S. FDA in 2010 states that the drug "may stop long bone growth in teenagers who are still growing."[33][D 5] Several reports state that premature epiphyseal closure can occur in acne patients receiving recommended doses of Accutane.[34][35][36][37]
Decreased night vision and keratoconjunctivitis sicca (dry eyes) has been reported to persist in some patients after discontinuation of isotretinoin therapy.[38][39][40]
Hyperostosis has been reported in patients receiving treatment with isotretinoin.[41][42]
Skin
The most common side effects are muco-cutaneous: dry lips and skin. Regular lip balm and moisturizer is recommended. Sometimes, however, the dose needs to be decreased to reduce these side effects.[43] The skin becomes more fragile—especially to frictional forces—and may not heal as quickly as normal. For this reason waxing of hair, tattooing, tattoo removal, piercings, dermabrasion, exfoliation, etc. are not recommended. Treatment of acne scars (e.g., with fractional laser such as "Fraxel") is generally deferred until 12 months after completion of a course of isotretinoin.
Acne usually flares up 2–3 weeks into the treatment and is usually mild and tolerable. Occasionally this flareup is severe, necessitating oral antiobiotics such as erythromycin. A short course of oral prednisolone may be required. Some dermatologists favour a few weeks pre-treatment with oral antibiotics before commencing isotretinoin to reduce the chance of a severe flare.
Teratogenicity
Isotretinoin is a teratogen highly likely to cause birth defects if taken by women during pregnancy or even a short time before conception. A few of the more common birth defects this drug can cause are hearing and visual impairment, missing or malformed earlobes, facial dysmorphism, and mental retardation. Isotretinoin is classified as FDA Pregnancy Category X and ADEC Category X, and use is contraindicated in pregnancy.[6]
The manufacturer recommends pregnancy be excluded in female patients two weeks prior to commencement of isotretinoin, and they should use two simultaneous forms of effective contraception at least one month prior to commencement, during, and for at least one month following isotretinoin therapy.[44]
In the U.S., more than 2,000 women have become pregnant while taking the drug between 1982 and 2003, with most pregnancies ending in abortion or miscarriage. About 160 babies with birth defects were born. As a consequence, the iPLEDGE program was introduced by the U.S. FDA on 12 August 2005 in an attempt to ensure female patients receiving isotretinoin do not become pregnant. As of 1 March 2006, only prescribers registered and activated in iPLEDGE are able to prescribe isotretinoin, and only patients registered and qualified in iPLEDGE will be able to have isotretinoin dispensed by a registered pharmacy. All patients, including women not of child-bearing age and men, must register with iPLEDGE. FDA's intent with the iPLEDGE program is to tightly control the distribution and dispensing of isotretinoin and thereby prevent the potential for distribution or sharing of the drug outside of the program to women of child-bearing age. In 2011, 155 pregnancies occurred among 129,544 women of childbearing potential taking isotrentinoin (0.12%)[45]
Patients receiving isotretinoin therapy are not permitted to donate blood during and for at least one month after discontinuation of therapy due to its teratogenicity.[46]
Psychological effects
The association between isotretinoin use and psychopathology has been controversial. Beginning in 1983, isolated case reports emerged suggesting mood change, particularly depression, occurring during or soon after isotretinoin use.[47] A number of studies have been conducted since then of the drug's effect on depression, psychosis, suicidal thoughts and other psychological effects.[47]
In 2012 a systematic review covering all articles in the literature related to isotretinoin, depression and suicide, as well as articles related to class effect, dose response, and biologic plausibility found that the literature reviewed was consistent with an association of isotretinoin administration and depression and with suicide in a subgroup of vulnerable individuals.[48] Following this systematic review, in a 2014 review a group of Australian dermatologists and psychiatrists collaborated on a set of recommendations for safe prescribing of isotretinoin.[49] However, whether isotretinoin use is causally associated with mental illness remains controversial.[49]
Mechanism of action
Isotretinoin's exact mechanism of action is unknown, but several studies have shown that isotretinoin induces apoptosis (cell death) in various cells in the body. Cell death may be instigated in the meibomian glands,[50][51] hypothalamic cells,[52] hippocampus cells[53][54] and—important for treatment of acne—in sebaceous gland cells.[55][56] Isotretinoin has a low affinity for retinoic acid receptors (RAR) and retinoid X receptors (RXR), but may be converted intracellularly to metabolites that act as agonists of RAR and RXR nuclear receptors.[4]
One study suggests the drug amplifies production of neutrophil gelatinase-associated lipocalin (NGAL) in the skin, which has been shown to reduce sebum production by inducing apoptosis in sebaceous gland cells, while exhibiting an antimicrobial effect on Propionibacterium acnes.[57][58][59] The drug decreases the size and sebum output of the sebaceous glands.[60] Isotretinoin is the only available acne drug that affects all four major pathogenic processes in acne, which distinguishes it from alternative treatments (such as antibiotics) and accounts for its efficacy in severe, nodulocystic cases.[61] The effect of Isotretinoin on sebum production can be temporary,[62] or remission of the disease can be "complete and prolonged."[60][63][64]
Isotretinoin has been speculated to down-regulate the telomerase enzyme and hTERT, inhibiting "cellular immortalization and tumorigenesis."[65] In a 2007 study, Isotretinoin was proven to inhibit the action of the metalloprotease MMP-9 (gelatinase) in sebum without any influence in the action of TIMP1 and TIMP2 (the tissue inhibitors of metalloproteases).[66] It is already known that metalloproteases play an important role in the pathogenesis of acne.[67]
Pharmacokinetics
Oral Isotretinoin is best absorbed when taken with a high-fat meal, because it has a high level of lipophilicity.[68] The efficacy of isotretinoin doubles when taken after a high-fat meal compared to when taken without food.[69] Due to Isotretinoin's molecular relationship to Vitamin A, it should not be taken with Vitamin A supplements due to the danger of toxicity through cumulative overdosing.[70] Accutane also negatively interacts with tetracycline, another class of acne drug, and with micro-dosed ('mini-pill') progesterone preparations, norethindrone/ethinyl estradiol ('OrthoNovum 7/7/7'), St. John's Wort, Phenytoin, and systemic corticosteroids.
Isotretinoin is primarily (99.9%) bound to plasma proteins, mostly albumin. Three metabolites of Isotretinoin are detectable in human plasma after oral administration: 4-oxo-isotretinoin, retinoid acid (tretinoin), and 4-oxo-retinoic acid (4-oxo-tretinoin). Isotretinoin also oxidizes, irreversibly, to 4-oxo-isotretinoin—which forms its geometric isomer 4-oxo-tretinoin. After an orally-administered, 80 mg dose of liquid suspension 14C-isotretinoin, 14C-activity in blood declines with a half-life of 90 hours.[68] The metabolites of isotretinoin and its conjugates are then excreted in the subject's urine and faeces in relatively equal amounts.[68] After a single, 80 mg oral dose of Isotretinoin to 74 healthy adult subjects under fed conditions, the mean ±SD elimination half-life (t1/2) of isotretinoin and 4-oxo-isotretinoin were 21.0 ± 8.2 hours and 24.0 ± 5.3 hours, respectively.[68] After both single and multiple doses, the observed accumulation ratios of isotretinoin ranged from 0.90 to 5.43 in patients with cystic acne.[68]
History
The compound 13-cis retinoic acid was first studied in the 1960s at Roche Laboratories in Switzerland by Werner Bollag as a treatment for skin cancer. Experiments completed in 1971 showed that the compound was likely to be ineffective for cancer and, surprisingly, that it could be useful to treat acne. They also showed that the compound was likely to cause birth defects, and in light of the events around thalidomide so Roche abandoned the product. In 1975, Gary Peck and Frank Yoder independently rediscovered the drug's use as a treatment of cystic acne while studying it as a treatment for lamellar ichthyosis, and published that work. Roche resumed work on the drug, In clinical trials, subjects were carefully screened to avoid including women who were or might become pregnant. Roche's New Drug Application for isotretinoin for the treatment of acne included data showing that the drug caused birth defects in rabbits. The FDA approved the application in 1982.
Scientists involved in the clinical trials published articles warning of birth defects at the same time the drug was launched in the US, but nonetheless isotretinoin was taken up quickly and widely, both among dermatologists and general practitioners. Cases of birth defects showed up in the first year, leading the FDA to begin publishing case reports and to Roche sending warning letters to doctors and placing warning stickers on drug bottles, and including stronger warnings on the label. Lawsuits against Roche started to be filed. In 1983 the FDA's advisory committee was convened and recommended stronger measures, which the FDA took and were that time unprecedented: warning blood banks not to accept blood from people taking the drug, and adding a warning to the label advising women to start taking contraceptives a month before starting the drug. However use of the drug continued to grow, as did the number of babies born with birth defects. In 1985 the label was updated to include a boxed warning. In early 1988 the FDA called for another advisory committee, and FDA employees prepared an internal memo estimating that around 1,000 babies had been born with birth defects due isotretinoin, that up to around 1,000 miscarriages had been caused, and that between 5,000 and 7,000 women had had abortions due to isotretinoin. The memo was leaked to the New York Times[71] a few days before the meeting, leading to a storm of media attention. In the committee meeting, dermatologists and Roche each argued to keep the drug on the market but to increase education efforts; pediatricians and the CDC argued to withdraw the drug from the market. The committee recommended to restrict physicians who could prescribe the drug and to require a second opinion before it could be prescribed. The FDA, believing it did not have authority under the law to restrict who had the right to prescribe the drug, kept the drug on the market but took further unprecedented measures: it required to Roche to make warnings yet more visible and graphic, provide doctors with informed consent forms to be used when prescribing the drug, and to conduct follow up studies to test whether the measures were reducing exposure of pregnant women to the drug. Roche implemented those measures, and offered to pay for contraception counseling and pregnancy testing for women prescribed the drug - the program was called the "Pregnancy Prevention Program".
A CDC report published in 2000[72] showed problems with the Pregnancy Prevention Program and showed that the increase in prescriptions was from off-label use, and prompted Roche to revamp its program, renaming it the "Targeted Pregnancy Prevention Program" and adding label changes like requirements for two pregnancy tests, two kinds of contraception, and for doctors to provide pharmacists with prescriptions directly; providing additional educational materials, and providing free pregnancy tests. The FDA had another advisory meeting in late 2000 that again debated how to prevent pregnant women from being exposed to the drug; dermatologists testified about the remarkable efficacy of the drug, the psychological impact of acne, and demanded autonomy to prescribe the drug; others argued that the drug be withdrawn or much stricter measures be taken. In 2001 the FDA announced a new regulatory scheme called SMART (the System to Manage Accutane Related Teratogenicity) that required Roche to provide defined training materials to doctors, and for doctors to sign and return a letter to Roche acknowledging that they had reviewed the training materials, for Roche to then send stickers to doctors, which doctors would have to place on prescriptions they give patients after they have confirmed a negative pregnancy test; prescriptions could only be written for 30 days and could not be renewed, thus requiring a new pregnancy test for each prescription.[citation needed]
In February 2002, Roche's patents for isotretinoin expired, and there are now many other companies selling cheaper generic versions of the drug. On June 29, 2009, Roche Pharmaceuticals, the original creator and distributor of isotretinoin, officially discontinued both the manufacture and distribution of their Accutane brand in the United States due to what the company described as business reasons related to low market share (below 5%), coupled with the high cost of defending personal-injury lawsuits brought by some patients prescribed the drug. Generic isotretinoin will remain available in the United States through various manufacturers. Roche USA continues to defend Accutane and claims to have treated over 13 million patients since its introduction in 1982. F. Hoffmann-La Roche Ltd. apparently will continue to manufacture and distribute Roaccutane outside of the United States.[73]
Among others, actor James Marshall sued Roche over allegedly Accutane-related disease that resulted in removal of his colon.[74] The jury, however, decided that James Marshall had a pre-existing bowel disease.[75]
Several trials over inflammatory bowel disease claims have been held in the United States thus far, with many of them resulting in multimillion dollar judgments against the makers of isotretinoin.[76] In 2009 Roche decided to pull Accutane off the market, stating at the time that the move was related to market pressures and the high cost of defending Accutane lawsuits.[77]
See also
References
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Epuris by Cipher Pharmaceuticals
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ 4.0 4.1 Lua error in package.lua at line 80: module 'strict' not found.
- ↑ 5.0 5.1 Lua error in package.lua at line 80: module 'strict' not found.[page needed]
- ↑ 6.0 6.1 6.2 6.3 Klasco RK, editor. Drugdex system, vol. 128. Greenwood Village (CO): Thomson Micromedex; 2006.[page needed]
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ 10.0 10.1 Choi JS, Koren G, Nulman I. Pregnancy and isotretinoin therapy. CMAJ. 2013 Mar 19;185(5):411-3. doi: 10.1503/cmaj.120729. PMID 23296582. PMC 3602257
- ↑ Joint Formulary Committee. British National Formulary. 47th ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain. ISBN 0-85369-584-9[page needed]
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Specifically, doctors who are fellows of the Australasian College of Dermatologists (FACD); cf. Pharmaceutical Services Branch, Guide to poisons and therapeutic goods legislation for medical practitioners and dentists, Sydney: NSW Department of Health; 2006.[page needed]
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ United States Pharmacopeia Staff. Consumer Reports Complete Drug Reference. Yonkers, NY: Consumer Reports Books, 1995. Pg 998.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ NetDoctor.co.uk / Roaccutane
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Roche Products Pty Ltd. Roaccutane (Australian Approved Product Information). Dee Why (NSW): Roche; 2005.[page needed]
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ BNF, edition 57[page needed]
- ↑ 47.0 47.1 Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ 49.0 49.1 Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Isotretinoin’s Mechanism of Action Elucidated. Medconnect (2009-08-28). Retrieved on 2010-11-13.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ 60.0 60.1 Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ [unreliable medical source?]Lua error in package.lua at line 80: module 'strict' not found.
- ↑ [unreliable medical source?]Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.[unreliable medical source?]
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ 68.0 68.1 68.2 68.3 68.4 Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Gina Kolata for the New York Times. April 22, 1988 Anti-Acne Drug Faulted in Birth
- ↑ CDC. January 21, 2000 Accutane®-Exposed Pregnancies -- California, 1999 MMWR Weekly 49(02);28-31
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
- ↑ Lua error in package.lua at line 80: module 'strict' not found.
Drugs@FDA references
The following are queries against the Drugs@FDA database used as references.
- ↑ For Roche's Accutane see database query run 3 August 2014.
- ↑ For Mylan's Amnesteem see database query run 3 August 2014.
- ↑ For Teva's Claravis see database query run 3 August 2014.
- ↑ For Ranbaxy's Absorica see database query run 2 August 2014.
- ↑ Label and approval history for Roche's Accutane, retrieved 3 August 2014.
External links
- Drugs.com Isotretinoin Information
- Dermatology Vol 9: issue 5: Night blindness, vitamin A deficiency, and isotretinoin psychotoxicity
- DermNet treatments/isotretinoin
- Wikipedia articles needing page number citations from October 2010
- Wikipedia articles needing page number citations from May 2012
- Articles lacking reliable references from August 2013
- Articles lacking reliable references from April 2012
- Chemical articles having calculated molecular weight overwritten
- Infobox drug articles without a structure image
- Articles with unsourced statements from August 2013
- Articles with unsourced statements from December 2015
- Retinoids
- Anti-acne preparations