Sacrotuberous ligament
| Sacrotuberous ligament | |
|---|---|

Articulations of pelvis, anterior view, with greater sciatic foramen (labeled in red) and its boundaries.
|
|
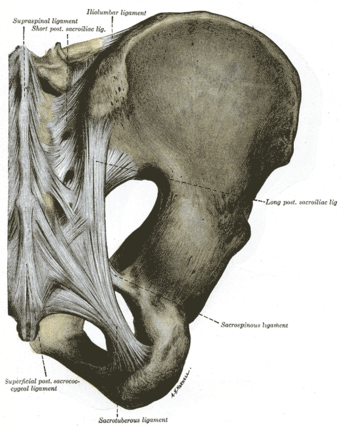
Articulations of pelvis. Posterior view.
|
|
| Details | |
| Latin | ligamentum sacrotuberale |
| From | sacrum |
| To | tuberosity of the ischium |
| Identifiers | |
| TA | Lua error in Module:Wikidata at line 744: attempt to index field 'wikibase' (a nil value). |
| TH | {{#property:P1694}} |
| TE | {{#property:P1693}} |
| FMA | {{#property:P1402}} |
| Anatomical terminology
[[[d:Lua error in Module:Wikidata at line 863: attempt to index field 'wikibase' (a nil value).|edit on Wikidata]]]
|
|
The sacrotuberous ligament (great or posterior sacrosciatic ligament) is situated at the lower and back part of the pelvis. It is flat, and triangular in form; narrower in the middle than at the ends.
Contents
Structure
It runs from the sacrum (the lower transverse sacral tubercles, the inferior margins sacrum and the upper coccyx[1]) to the tuberosity of the ischium.
The sacrotuberous ligament is attached by its broad base to the posterior superior iliac spine, the posterior sacroiliac ligaments (with which it is partly blended), to the lower transverse sacral tubercles and the lateral margins of the lower sacrum and upper coccyx. Its oblique fibres descend laterally, converging to form a thick, narrow band that widens again below and is attached to the medial margin of the ischial tuberosity. It then spreads along the ischial ramus as the falciform process, whose concave edge blends with the fascial sheath of the internal pudendal vessels and pudendal nerve. The lowest fibres of gluteus maximus are attached to the posterior surface of the ligament; superficial fibres of the lower part of the ligament continue into the tendon of biceps femoris. The ligament is pierced by the coccygeal branches of the inferior gluteal artery, the perforating cutaneous nerve and filaments of the coccygeal plexus.[2]
Variation
The membranous falciform process of the sacrotuberous ligament was found to be absent in 13% of cadavers. When present it extends towards the ischioanal fossa travelling along the ischial ramus and fusing with the obturator fascia.
The lower border of the ligament was found to be directly continuous with the tendon of origin of the long head of the Biceps femoris in approximately 50% of subjects.[3] Biceps femoris could therefore act to stabilise the sacroiliac joint via the sacrotuberous ligament.
Function
The sacrotuberous ligament contains the coccygeal branch of the inferior gluteal artery.
Clinical significance
If the pudendal nerve becomes entrapped between this ligament and the sacrospinous ligament causing perineal pain, the sacrotuberous ligament is surgically severed to relieve the pain.
Additional images
-
Gray1243.png
Nélaton’s line and Bryant’s triangle.
External links
- Anatomy figure: 13:03-04 at Human Anatomy Online, SUNY Downstate Medical Center - "Deep muscles of the gluteal region with gluteus medius and maximus muscles removed."
- Anatomy figure: 17:02-05 at Human Anatomy Online, SUNY Downstate Medical Center - "Posterior view of the bones and ligaments of the hip joint."
- Anatomy photo:41:os-0114 at the SUNY Downstate Medical Center - "The Female Perineum"
- Anatomy photo:42:12-0102 at the SUNY Downstate Medical Center - "The Male Perineum and the Penis: Boundaries of the Ischioanal fossa"
- Anatomy image:9075 at the SUNY Downstate Medical Center
- hip/hip%20ligaments/ligaments7 at the Dartmouth Medical School's Department of Anatomy
References
This article incorporates text in the public domain from the 20th edition of Gray's Anatomy (1918)
- ↑ Marios Loukas,Robert G Louis Jr, Barry Hallner, Ankmalika A Gupta and Dorothy White. (2006) "Anatomical and surgical considerations of the sacrotuberous ligament and its relevance in pudendal nerve entrapment syndrome" Surg Radiol Anat 28(2): 163-169
- ↑ Gray's anatomy, 40 edition.
- ↑ Vleeming, A., R. Stoeckart, et al. (1989). "The sacrotuberous ligament: a conceptual approach to its dynamic role in stabilizing the sacroiliac joint." Clinical Biomechanics 4(4): 200-203.


