Abstract
The steep rise of type 2 diabetes mellitus (T2DM) and associated complications go along with mounting evidence of clinically important sex and gender differences. T2DM is more frequently diagnosed at lower age and body mass index in men; however, the most prominent risk factor, which is obesity, is more common in women. Generally, large sex-ratio differences across countries are observed. Diversities in biology, culture, lifestyle, environment, and socioeconomic status impact differences between males and females in predisposition, development, and clinical presentation. Genetic effects and epigenetic mechanisms, nutritional factors and sedentary lifestyle affect risk and complications differently in both sexes. Furthermore, sex hormones have a great impact on energy metabolism, body composition, vascular function, and inflammatory responses. Thus, endocrine imbalances relate to unfavorable cardiometabolic traits, observable in women with androgen excess or men with hypogonadism. Both biological and psychosocial factors are responsible for sex and gender differences in diabetes risk and outcome. Overall, psychosocial stress appears to have greater impact on women rather than on men. In addition, women have greater increases of cardiovascular risk, myocardial infarction, and stroke mortality than men, compared with nondiabetic subjects. However, when dialysis therapy is initiated, mortality is comparable in both males and females. Diabetes appears to attenuate the protective effect of the female sex in the development of cardiac diseases and nephropathy. Endocrine and behavioral factors are involved in gender inequalities and affect the outcome. More research regarding sex-dimorphic pathophysiological mechanisms of T2DM and its complications could contribute to more personalized diabetes care in the future and would thus promote more awareness in terms of sex- and gender-specific risk factors.
Introduction
-
Biological Risk Factors
Body mass index (BMI)
Body fat distribution
Brown adipose tissue (BAT)
Metabolic syndrome (MetS)
Adipokines
New biomarkers
Imbalance of sex hormones
Prediabetes
Gestational Diabetes Mellitus (GDM)
-
Psychosocial Risk Factors
Socioeconomic status
Psychosocial stress
Sleep deprivation and work stress
-
Health Behavior
Lifestyle
Sugar-sweetened beverages (SSBs)
Alcohol
Smoking
-
Pathophysiological Mechanisms With Sexual Dimorphism
Developmental origins of health and disease
Fetal programming/epigenetics in animals
Fetal programming/epigenetics in humans
Fetal sex and risk for GDM
Neonatal fat distribution
Small or large for gestational age neonates
Endocrine disruptors
Genetic predisposition
Gonosomes
Glucose tolerance
Insulin sensitivity and secretion
Incretin hormones
Gastric emptying and glucose absorption
Ectopic fat
Energy imbalance
HPA axis activity and stress model
Hypothalamic melanocortin system
-
Cardiovascular Complications
Risk factors
Coronary heart disease
Coagulation
Cardiac energy supply
Mortality
Cardiomyopathy
Diabetic Foot Syndrome
Diabetic Nephropathy
-
Other Frequent Comorbidities
Functional limitations
Mental disorders
Sexual function and reproduction
Future Perspective
Conclusions
I. Introduction
There is increasing evidence that sex and gender differences are important in epidemiology, pathophysiology, treatment, and outcomes in many diseases, but they appear to be particularly relevant for noncommunicable diseases. Many organizations now call for the inclusion of the sex and gender dimension in biomedical research, to improve the scientific quality and societal relevance of the produced knowledge, technology, and/or innovation (1). In the domain of endocrinology and metabolism, the greatest body of evidence for important clinical implications of sexual dimorphisms comes from studies in the field of type 2 diabetes mellitus (T2DM). Genetic background, lifestyle, and environment contribute to the pandemic increase of T2DM and its associated complications (Figure 1), presenting a challenge for healthcare systems (2). Therefore, this review will provide important but often unrecognized knowledge on sex and gender differences in T2DM, to increase awareness of all health professionals and of all readers interested in endocrinology.
Figure 1.
Lifelong impact and interaction between sex and gender on development and outcomes of T2DM: social conditions (upper) and biological factors (lower) influence the development of germ cells, fetal programming, the newborn, puberty, reproductive age, ageing, and the manifestation of T2DM in men and women as well as the progression of its complications and comorbidities. Modified from Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes, by EUGenMed Cardiovascular Clinical Study Group, Regitz-Zagrosek V, Oertelt-Prigione S, et al. Eur Heart J. 2016;37:24–34 with permission.
Sex differences describe biology-linked differences between women and men, which are caused by differences in sex chromosomes, sex-specific gene expression of autosomes, sex hormones, and their effects on organ systems (Figure 1) (1, 3). Women show more dramatic changes in hormones and body due to reproductive factors during lifetime.
Gender differences arise from sociocultural processes, such as different behaviors of women and men, exposition to specific influences of the environment, different forms of nutrition, life styles or stress, or attitudes towards treatments and prevention (Figure 1) (1, 3). It also has to be noticed that the parameters, sex or gender, are not straight forward binary categories and that a multiple of femininities or masculinities converge with other important sociodemographic variables (4). In addition, gender roles and gender identity are influenced by a complex interplay between genetic, endocrine, and social factors (5). Sex hormones affect behavior during the whole life and physical changes can have implications on lifestyle, social roles, and on mental health. Moreover, the environment influences biology via epigenetic mechanisms (Figure 1). As demonstrated by endocrine disruptors, strong abilities to modulate biological phenotypes in a sex-specific manner are possible. Thus, most findings in chronic diseases are influenced by a combination of biological and environmental factors, verifying that there are many interactions of societal and biological factors in women and men (6). Sex and gender differences are equally important in development, awareness, presentation, diagnosis, and therapy, as well as prevention of the lifestyle-associated disease T2DM (Figure 1). This review will address biological differences in hormones, body composition, glucose and fat metabolism, reproduction, and some pathophysiologic sex-dimorphic mechanisms, as well as gender differences in education, income, social support, and lifestyle in the risk and outcome development of T2DM. Major diabetic complications will be discussed with emphasis on known sexual dimorphism and gender differences will focus on cardiovascular disease (CVD), cardiomyopathy, and nephropathy. However, always making an accurate distinction between “sex” and “gender” effects is almost impossible, because these 2 complex processes are interrelated and interact with each other during lifetime. On the basis of all these facts, in this review, sex will be used to indicate primarily biological differences and gender to describe predominant psychosocial influences. However, a clear judgement is often not possible and manifold interactions between biological and societal influences, in the development and clinical outcome of T2DM, always have to be kept in mind.
The great impact of psychosocial risk factors on top of biological ones are visualized by the marked regional differences and trajectories of prevalence rates of T2DM in adult men and women (Figure 2A). Overall, age dependency is evident in both sexes with small differences in age-specific prevalence based on global estimates (Figure 2B). In 2013, the proportion of overweight females has increased to 38%, which is very similar to that in men (37%). However, according to a systematic analysis females tend to be more obese than men (2). In addition, more women are overweight or obese after the age of 45 years, whereas more males are overweight at younger age (Figure 2C). Larger sex differences in obesity rates were reported in countries with greater gender inequality, quantitatively assessed by the global gender gap index, and the gender inequality index in multicountry ecological studies (7–9). The dimension of female obesity was found to be greater in countries characterized by gender inequality, derived by social or economic data (7). A strong inverse association between a comprehensive measure of income-based socioeconomic inequality and obesity was found among young white women, in a cross-sectional representative multiethnic sample of the United States population (10). Furthermore, income inequality was related to the rates of obesity and of diabetes mortality in developed countries in both sexes, with stronger effects in women (8). In females, the effect of income inequality on obesity was also independent of average caloric consumption (8). Because obesity is the major risk factor of T2DM in both sexes, it is not surprising that the prevalence patterns of T2DM across regions resemble those of obesity. Nevertheless, globally more males are diagnosed with diabetes. In 2013, there were 14 million times more men affected with diabetes than women (11). More than half of the diabetic subjects are middle aged, and incidence rises with increasing ages in both sexes, reaching highest rates in the very old women (Figure 2B). Besides impaired glucose tolerance (IGT) is more common in females than males independent of age (Figure 2B). Most patients with T2DM live in low- and middle-income countries, but prevalence rates are higher in high-income countries, where lower socioeconomic groups are disproportionally affected. Striking sex and regional differences in the increase of obesity-related T2DM prevalence developed throughout the last 3 decades, reflecting complex relationships with differences in ethnicity, migration, culture, lifestyle, gene-environment interactions, socioeconomic status (SES) and social roles (12). Overall, highest growth was described in Oceania for both sexes, followed by South and Central Asia, Middle East, and North Africa for women, and in the high income dominated Asia-Pacific and Western region for men (12). In Belize, the prevalence doubled in women compared with men, following robust results derived from both self-reporting and blood glucose measurements (12). However, such global estimates of sex differences also have limitations, which may be due to random testing, selection bias, and sex disparities in access to healthcare in some countries.
Figure 2.
Prevalence of prediabetes, diabetes, and overweight/obesity in men and women. A, Percent of women (pink) and men (blue) (age 25+) with fasting glucose more than or equal to 126 mg/dL (7.0 mmol/L) or on medication for raised blood glucose (age-standardized estimate) in 2014 (348). B, Prevalence of IGT and diabetes by age and sex in 2013 (11). C, Prevalence of overweight and obesity by age and sex in 2013 (2).
For review criteria, the PubMed database was searched for full-text articles published between the period of January 1, 2004 and February 24, 2016. The search terms used were sex or gender in combination with “diabetes” within the article title. Results were screened for relevant articles. The authors contributed further articles to the search results based on their personal knowledge and experience.
II. Biological Risk Factors
A. Body mass index (BMI)
Important physiological and pathophysiological sex differences of anthropometric, metabolic, and endocrine parameters are summarized in Figure 3. A short overview of the most interesting risk factors and markers are presented in Table 1.
Figure 3.
Overview of physiological and pathological sex differences in metabolism and energy homeostasis in men (left) and women (right). Blue arrows indicate higher or lower levels or impact in men compared with women. Red arrows indicate higher or lower levels or impact in women compared with men. Fat mass: red, SAT; orange, VAT; purple, BAT. ARC POMC, arcuate nucleus POMC; FFA, free fatty acid; RR, relative risk. These facts are described in more detail in the main text, eg, in the sections II and V, respectively.
Table 1.
Sex Dimorphism in Diabetes Risk Factors
| Risk Factors | Diabetes Risk |
Notes | Reference | |
|---|---|---|---|---|
| Men | Women | |||
| BMI | + | + | Men: diabetes diagnosis at lower BMI | 9, 13, 15, 18, 25 |
| Stronger obesity-diabetes risk association in women | ||||
| Better predictor of T2DM in men | ||||
| WCR | + | ++ | Better predictor of T2DM in women | 23–25 |
| More prominent increase with increasing age in women | ||||
| Clustering of metabolic risk factors, MetS | + | + | Similar prevalence but sex-dimorphic clustering of risk factors: higher prevalence of hypertension and adiposity in women and of low HDL-cholesterol and higher uric acid levels in males; in younger subjects, the combination of dyslipidemia with increased WCR was most prevalent in females but with hypertension in males | 34–36 |
| No-leisure time physical activity (LTPA) | + | ++ | Greater impact on obesity and closer association with increased abdominal adiposity in women than men | 119–123 |
| Prediabetes | + | + | 82 | |
| IFG | ++ | + | Men: More often (isolated) impaired fasting glucose (highest rates, 50–70 y) | |
| IGT | + | ++ | Women, more often (isolated) IGT (until 80 y) | |
| Higher testosterone | − | + | Metaanalysis: 60% higher diabetes risk in women, 42% lower diabetes risk in men | 71 |
| Sexual-dimorphic risk of hyperandrogenism | ||||
| Low SHBG | + | ++ | Stronger association with diabetes risk in women | 60, 61 |
| SHBG gene polymorphisms relate to diabetes risk | ||||
| Hyperinsulinemia and increased liver fat strongly relate to low circulating SHBG | ||||
| Previous GDM | n.a. | ++ | 71% higher incidence of T2DM among prediabetic women | 85, 86 |
| Metaanalysis: 7-fold greater risk of development of T2DM compared with women who maintained NGT during pregnancy | ||||
| PCOS | n.a. | 2+ | 4-fold higher risk for T2DM | 73 |
| Shift work (related to sleep deprivation) | Overall, controversial results, sex-dimorphic impact of chronotypes | |||
| ++ | + | Greater diabetes risk in men in a metaanalysis | 106–108 | |
| + | ++ | Greater diabetes risk in women in other studies: in women, BMI mainly influenced the association with T2DM | 103–105 | |
| Greater association of night-work exposure and incident T2DM in women in some studies | ||||
| Job strain | ||||
| High work demands | − | 0 | Protective in men | 100 |
| Low decision latitude | 0 | + | Higher diabetes risk in women, particularly greater in combination with high demands | 100 |
| High straina | 0 | + | Lower diabetes risk in nonobese men and higher diabetes risk in obese women | 100–102 |
| Active jobb | − | 0 | Protective in men | 100 |
| Low education | 0 | + | Higher diabetes risk in women | 93 |
| High occupation | 0 | − | Occupation, women's autonomy, and empowerment appear more protective against obesity for women than education on its own | 95, 349 |
| Low SES | + | ++ | Inverse association between SES and prevalence of obesity and diabetes in developed countries with stronger association in women, especially in white young women | 10 |
| Low childhood SES | 0 | + | 98 | |
| Smoking | + | + | Comparably increased diabetes risk, but 25% greater increase of cardiovascular risk in women | 134, 138 |
0, no effect; −, decreases diabetes risk; +, increases diabetes risk; ++, increases diabetes risk to a greater extent; n.a., nonappropriate.
High demand with low decision latitude.
High demand with high decision latitude.
Across the age range, European men are usually diagnosed with diabetes at an earlier age (Figure 2B) and at lower BMI than women, with the most prominent sex difference being at younger age (13). In Sweden, time trends revealed that the male predominance in 1940, with a male to female ratio up to 1.4 in the ages 10–55 years, increased and expanded over time especially in the age group 45–65 years reaching a ratio of 2 (14). Men were diagnosed 3–4 years earlier and at a BMI 1–3 kg/m2 lower. This trend was partly explained by an increase of automation and decrease of physical work particularly in men. Diabetic women, on the other hand, are more obese than diabetic men in most studies and show a stronger association between increase of BMI and diabetes risk, despite similar curvilinear associations between increasing BMI and diabetes risk in both sexes (15). Sex differences in body composition and fat deposition clearly contribute to sex-dimorphic diabetes risk (16). BMI overestimates body fat mass in men, who generally have more fat-free muscle compared with women.
B. Body fat distribution
During puberty, increased accumulation of gluteo-femoral fat promoted by estrogen results in a “gynoid shape” of premenopausal women (Figures 3 and 4). Males feature a greater trunk and visceral fat (VAT), upper extremity mass, and liver fat compared with females with same age and BMI (16, 17). Nonetheless, men and women with similar degree of insulin resistance show comparable intraabdominal and liver fat (18). In an Asian population, women with normal waist circumference (WCR) and BMI were diagnosed with visceral obesity by computer tomography. This even showed greater cardiometabolic risk in women, in terms of glucose and lipid abnormalities compared with males (19). However, VAT and age were independent predictors of greater cardiometabolic risk in males, whereas the VAT to subcutaneous fat (SAT) ratio independently predicted higher risk in females.
Figure 4.
Sex differences in fat distribution. MR image showing area between L5 and L4 at the lumbar spine in a male and female young healthy, normal-weight subject of comparable age and BMI (A and B) and a male and female patient with T2DM of comparable age and BMI (C and D). A, Man, 23 years old, BMI 25 kg/m2, VAT from area L2 to L5 216 cm2, SAT 649 cm2, liver fat 1.9%. B, Woman, 19 years old, BMI 24 kg/m2, VAT from area L2 to L5 138 cm2, SAT 807 cm2, liver fat 1.1%. C, Man, 59 years old, BMI 33, VAT from area L2 to L5 901 cm2, sc 879 cm2, liver fat 9.6%. D, Woman, 57 years old, BMI 34, VAT from area L2 to L5 712 cm2, SAT 2158 cm2, liver fat 5.1%.
In general, men not only featured larger amounts of VAT for any degree of total body fat but also higher levels of fatty acids (FAs) turnover with higher rates of lipolysis and lipogenesis in VAT compared with women (20). Women, instead, have higher rates of FA uptake in leg fat tissue and lower rates of release in gluteal and femoral regions. Also females expressed higher lipogenetic rates from SAT compared with males. Increased leg adiposity was found to be associated with a decreased cardiometabolic risk especially in women, whereas higher trunk adiposity is generally related to clustering of cardiometabolic risk factors in cross-sectional population-based studies (21, 22). Aging and in particular menopause transition, with loss of estrogen production, is associated with changes in body shape and a preferential increase of abdominal fat in women shifting to the android “visceral adiposity” (23).
In line with this, women have a more prominent increase of WCR with increasing age than men. The relationship between WCR and intraabdominal fat mass is stronger for intraabdominal SAT in younger women than men; but in menopausal women, the associations become more similar to the male patterns in cross-sectional analysis testing for sex and age differences (24). In British elder subjects waist was the best predictor of diabetes in women, whereas in males the predictive value of BMI and waist were comparable (25). These results are confirmed by data from various other cohorts from different countries (26, 27) and further expanded by trajectories of anthropometric parameters. In pooled analysis of 2 prospective population-based cohort studies, German women who gained 1 cm of their WCR had an increased risk for incident diabetes of 31% per year, compared with 28% if they gained 1-kg body weight (28). In men, the corresponding increase of risk for incident diabetes was 29% and 34%.
C. Brown adipose tissue (BAT)
Sex differences are described regarding mass and activity of BAT in adults (Figure 3), which was recently supposed to impact whole-body energy metabolism, insulin resistance, and obesity-related T2DM. Women have much higher prevalence and activity of BAT, which was related independently and inversely to age in both sexes, but only to BMI in males and only to VAT in females, in a large population-based study (29). In mice, expression of factors involved in BAT activity, like fibroblast growth factor families, was positively regulated by the presence of ovaries and estrogens (30). BAT transplantation reversed obesity, increased adiponectin, and reduced insulin resistance and liver steatosis in leptin-deficient animals (31). Therefore, overall higher impact of BAT could also contribute to lower diabetes risk in women.
D. Metabolic syndrome (MetS)
Clustering of traditional metabolic risk factors associated with insulin resistance, often termed MetS, disregard risk factors like age, sex, family history, SES, and lifestyle. Recent analysis of National Health and Nutrition Examination Survey data show comparable prevalence in both sexes with greatest increase in young women (32). Diabetes appears to diminish the in general more favorable cluster of risk factors of females compared with males, leading to greater differences in central adiposity and risk factors related to coagulation and inflammation between diabetes and nondiabetes in women rather than in men (33). Clustering of risk factors varies between sexes and ethnicities, but abdominal obesity and increased WCR as surrogate markers seem to be the dominant factors in women (34–36). Overall, adjustment of risk factors for MetS appears to have greater impact on women's CVD risk. There are several diabetes risk scores, including sex in risk calculations together with various other risk parameters, but only a few include WCR or social factors like social deprivation (37, 38).
As recently shown in a collaborative analysis of 10 large cohort studies, women appear to feature more often the metabolically healthy obese phenotype with normoglycemia and without dyslipidemia and hypertension (7%–28%) compared with males (2%–19%) (39). As demonstrated by a recent metaanalysis of prospective cohort studies even obese men and women with normal cardiometabolic clustering had a 4-fold higher relative risk of developing T2DM, although this risk was only half of that of metabolically unhealthy obese patients regardless of sex differences in the progression toward T2DM (40).
E. Adipokines
Sexual dimorphism is also evident in the expression and the predictive value of some fat-related biomarkers (16, 41, 42). Leptin is important in the regulation of satiety, food intake, and energy expenditure. It also influences the insulin glucose axis as well as peripheral insulin resistance (43). Similarly, adiponectin has manifold effects on lipid and glucose metabolism and increases insulin sensitivity in target organs. Dysregulation of adiponectin action is relevant in the development of T2DM (44).
Women show an up-regulation of expression of adiponectin and its receptor in abdominal adipose tissue, possibly contributing to their lower cardiometabolic risk. In general, metaanalyses have shown that women have higher leptin and adiponectin levels than men of comparable age and BMI, which may be related to their sexual hormones (41, 45). In several longitudinal studies, increased plasma leptin, which mirrors body fat mass and is strongly associated to SAT, relates to increased diabetes risk in males (37). On the other hand, an inverse correlation between plasma adiponectin levels and insulin sensitivity is seen in obese and diabetic subjects, which tends to be somewhat more pronounced in women (45–47). In addition, androgens may decrease adiponectin secretion. However, it is still unclear whether hypoadiponectinemia is a cause or a consequence of insulin resistance or hyperinsulinemia (37).
F. New biomarkers
There are also a number of new risk factors reported with sexual dimorphism, such as the hepatokine fetuin A, which was shown to be related to T2DM onset only in women in the Rancho Bernardo Study (42). In the Prevention of Renal and Vascular Endstage Disease Study, copeptin, the C-terminal portion of the precursor of vasopressin and reliable marker of arginine vasopressin secretion, was shown to be associated with the risk of future diabetes in women but not in men (48). Inclusion of copeptin in risk models based on traditional risk factors was of additive value in predicting diabetes in women. This may point to a closer link between arginine vasopressin stress adaptation system and pathogenesis of T2DM in women. The development and validation of new risk scores with sex-specific weighting of risk factors could be a promising tool for future prediction models.
Another novel biomarker is proneurotensin, the precursor molecule of neurotensin, which is peripherally released from the endocrine-like N-cells of the small intestine after fat intake (49). It acts as neurotransmitter in the central nervous system but behaves as a hormone in the periphery, stimulating pancreatic and biliary secretion, inhibiting gastric motility, and facilitating FA translocation. Fasting proneurotensin plasma levels are usually lower in women than men but predict incident diabetes and CVD as well as total and cardiovascular mortality in women and, however, not in men (50). Each standard deviation increase of baseline proneurotensin was associated with an increased risk of 41% for new-onset diabetes in women during the follow-up of 13 years.
In a cross-sectional population-specific study, low 25(OH) vitamin D3 was found in middle-aged Caucasians independently associated with T2DM in women but not in men (51). A significant interaction between sex and vitamin D was found before sex-stratified analysis. The probability of having a newly diagnosed or known diabetes more than doubled in women with levels below a cut-off of 15 ng/mL. In men, seasonally adjusted values only marginally predicted T2DM. In a previous metaanalysis, an inverse association between vitamin D and diabetes was confirmed in both men and women (52). However, some differences between the studies could be explained by ethnicity and age as sex hormones, particularly 17α-estradiol, may influence these associations with variations over time (53). In fact, in the Korean population low levels were related to increased diabetes prevalence in younger women and older men over 50 years. Vitamin D may also directly stimulate the expression of the insulin receptor, thereby improving glucose transport in human cells (54).
In a large community-based prospective cohort study, increased liver enzymes (alanine aminotransferase, aspartate aminotransferase, and γ-glutamyl transferase [GGT]) preceded the incidence of T2DM in both sexes (55). The strongest association with incident T2DM was seen for GGT. This could be explained by the fact that GGT is more closely related to fatty liver, oxidative stress, and thus to insulin resistance compared with the other enzymes (55). The independent association between liver enzymes and diabetes risk was continuously extending in the normal range, hence it remained significant by use of sex-specific quartiles and showed no significant sex interaction overall. Women usually have lower levels and lower liver fat than men, of comparable BMI and age, and appear to be protected by estrogen at premenopausal age (56). Although overall males have a higher prevalence of increased liver fat, a marked rise is described in elder women (57). In a historical cohort of the Brisighella Heart Study, the fatty liver index, including liver enzymes, triglycerides, WCR, and BMI, was even a better predictor of the MetS in women than in men (58). Furthermore, a sex-specific association between liver transaminase levels and insulin sensitivity was described (59). Alanine aminotransferase independently predicted muscle glucose uptake measured by hyperinsulinemic euglycemic clamp in females only, whereas in males, fasting insulin and leptin were stronger predictors of insulin resistance.
Additionally, low sex hormone-binding globulin (SHBG) levels may indicate diabetes-risk potentially mediated via SHBG gene polymorphisms (60, 61). In general, women tend to have higher SHBG levels than men and low SHBG concentrations may be associated with even higher diabetes risk in women compared with men. In the Diabetes Prevention Program, SHBG and SHBG-single nucleotide polymorphisms did not predict incident diabetes in any sex, but diabetes incidence was directly associated with estradiol and estron and inversely with testosterone in men (62). Although not directly evaluated in this study, the association between circulating estrogen and diabetes risk could be attributed to systemic estrogen resistance in men (63). However, in this study, sex steroids did not relate to diabetes risk in women (62). The authors conclude that, although SHBG may be able to predict diabetes in unselected populations, in high-risk groups, elevated glucose and weight are more potent indicators of development of diabetes. However, in a large population-based sample, an independent inverse relationship was proven between SHBG and MetS, as well as incident T2DM, especially among postmenopausal women (64).
G. Imbalance of sex hormones
Cardiometabolic similarities were described among women with androgen excess and men with androgen deficiency. The balanced proportion between estrogens and androgens plays an important role in maintenance of energy metabolism, body composition, and sexual function. Also the bidirectional modulation of glucose and lipid homeostasis by sex hormones and their receptor activation in central and peripheral targets in both sexes are influenced by estrogens and androgens (16, 17, 65–69). In women, higher levels of androgens lead to increased body weight and VAT; this is also seen in female to male transsexuals (70). Overall, relatively higher testosterone levels in women and lower levels in men relate to incident diabetes (71).
The polycystic ovary syndrome (PCOS) describes a female-specific state of androgen excess and hyperinsulinemia related to obesity, T2DM, and higher cardiometabolic risk (72, 73). An influence of genetic aspects is supported by higher prevalence of metabolic disorders in both male and female. First-degree relatives of women with PCOS and impaired glucose metabolism (IGM) among men is strongly mediated by obesity (74). In addition, a sex difference in the parental metabolic phenotype was reported referring to fathers, which feature a higher risk of fasting dysglycemia and evidence for pancreatic β-cell secretory defects, when compared with mothers of women with PCOS. Nevertheless, only maternal heritability exerted a significant impact on the prevalence of fasting dysglycemia in these women (75).
Obese or diabetic males feature a 2- to 4-fold higher rate of late-onset hypogonadism with low testosterone levels and higher prevalence of erectile dysfunction (76, 77). Overweight/obese males showed accelerated aromatization of androgens to estrogens, inhibiting gonadotropin secretion by activation of estrogen receptors (ERs) of the hypothalamus that promote hypogonadism (78). Aromatization of testosterone to 17β-estradiol impacts energy homeostasis. A higher testosterone-estrogen ratio can promote visceral obesity in males, but androgen deficiency itself associates with increased VAT. Whether testosterone deficiency itself causes metabolic derangement or testosterone levels are decreased due to aging, changes of body composition, or illness (reverse causality) is not yet fully understood and needs further clarification (79, 80). However, testosterone replacement therapy can improve insulin sensitivity and hyperglycemia in hypogonadal diabetic males (81).
H. Prediabetes
The prevalence of prediabetic categories differ between sexes (Figure 2B) giving rise to clinical implications: men more often develop impaired fasting glucose (IFG), whereas women more often show IGT (Figure 2B). IFG is characterized by increased hepatic glucose output and impaired early insulin secretion, whereas IGT is primarily due to peripheral insulin resistance (82). IGT may better predict progression to diabetes and mortality risk relates more strongly to an increased cardiovascular risk. This fact may explain why World Health Organization criteria, including IGT status may be superior to other definitions of MetS in prediction of diabetes and CVD in women (83, 84). It further highlights the importance of performing oral glucose tolerance tests to screen for IGT, especially in women.
I. Gestational Diabetes Mellitus (GDM)
GDM is a heterogeneous entity were mostly insulin-resistant overweight/obese women are affected. It serves as an independent and strong female risk factor for eventual progression of T2DM (85). Nonetheless, normal weight women may also be susceptible to gestational diabetes (GDM) due to genetic traits, along with physiologically increasing insulin resistance during the course of pregnancy. Although intervention strategies might be an effective approach to reduce progression to T2DM, women with a history of GDM face a more than 70% higher incidence than prediabetic women do (86). Throughout literature, GDM is associated with several adverse pregnancy outcomes affecting not only mothers but also their offspring in a sex-specific way (87, 88). Recent studies report that pregnant women carrying a male fetus have higher risk for developing GDM (see section V.D) (89–91).
III. Psychosocial Risk Factors
Modifiable social factors, like low educational level, occupation, and income, largely contribute to unhealthy lifestyle behavior and social disparities and thus are related to higher risk of obesity and T2DM particularly in women (Table 1) (92, 93). In this context, it has to be emphasized that psychosocial risk factors and stress consist of economic, environmental, and behavioral components. These may differently influence diabetes risk overall and between men and women, but they are usually interrelated to each other. Further showing intricacy of this issue and limitations of many studies.
A. Socioeconomic status
SES, assessed by educational level, position, and income, is inversely associated with prevalence of obesity and T2DM in developed countries. Steeper gradients among women can be observed in a national population health survey in Canada (94). This study found persisting associations between low education and income and self-reported diabetes after controlling for obesity and physical activity in women. Consistently, a population-based European survey, the Kooperative Gesundheitsforschung in der Region Augsburg (KORA) study (95) found stronger associations between SES indicators, abdominal obesity, and physical activity in women. Additionally, a strong inverse association between occupation and newly detected diabetes was presented only in women (95). On the other hand, low SES, evaluated by occupation, relates to risk of IGT in men, independent of other confounders. Confirmed by a metaanalysis of case-control and cohort studies low SES is an important risk factor for T2DM in both sexes worldwide (96).
Furthermore, the application of a validated diabetes risk prediction algorithm in a nationally representative cross-sectional survey in Canada showed that among the individual level SES variables, such as lower household income and food insecurity, predicted a higher diabetes risk in women but not in men (97). On the other hand, a strong protective effect was found only for women living in ethnically dense areas, which is an area-level indicator of SES used by the Canadian Marginalization Index for ethnic concentration. In a longitudinal population-based study, childhood SES, assessed from fathers' occupation or education, was a robust predictor of incident diabetes, especially among women, which had a cumulative risk effect for both childhood SES and adult BMI (98). Higher levels of physical inactivity, energy intake, smoking, and stress factors enhance neuroendocrine perturbations in women compared with men with low SES. Conclusively, studies claim that women appear more sensitive to socio-contextual predictors, such as education, income, and occupation, for future diabetes risk development. This may be the cause due to multiple environmental and behavioral mechanisms; however, more studies are definitely needed to clarify this complex issue.
B. Psychosocial stress
Females appear to be more vulnerable to the adverse effects of cardiometabolic impact of psychosocial stress, occupational stress, and sleep disturbances as well as partly by unhealthy behavior (Table 1) (99–105). However, all together results are controversial (Table 1) (106–108). Greater amounts of unpaid housework and responsibilities in the family may contribute to feelings of conflicting demands and sustained stress levels in females, even in matched highly educated groups of employees (109, 110). Discrimination and gender roles may further increase the environmental psychosocial stress, as well as the stress responses especially in women. Besides, large geographical differences in countries, depending on culture and gender equality, were observed. The so-called “allostatic load,” ie, the imbalance between the ability to adapt to environmental demands and overexposure to environmental stress, increase the risk of cardiometabolic diseases via neuroendocrine, autonomic, and immune mediators (see section V.P) (111).
C. Sleep deprivation and work stress
Discrimination and posttraumatic stress disorders exert greater negative impact on sleep health in women rather than in men. In a sex-specific metaanalysis of epidemiological studies, women at all ages were shown to be at a 40% higher risk for suffering from insomnia (112). In turn, sleep loss, short-sleep duration, and impaired quality of sleep correlated with obesity and even more strongly with IGM related to insulin resistance (113). In the Nurses' Health study, a close link between less than 5 hours of sleep and incidence of hypertension was found in younger women (114), and sleep deprivation also exerted more detrimental cardiovascular effects among women in the Whitehall II cohort. This was, however, attenuated after correcting for other cardiovascular risk factors and depression in the prospective analysis (115). In a metaanalysis, both short sleep (<5 h) and difficulties initiating or maintaining sleep were associated with higher diabetes risk. However, comparable effect estimates were observed in both sexes after stratification by sex (116). In one smaller prospective study looking for sex differences as primary outcome, sleep deprivation led to increased food and fat intake; however, males were more susceptible to weight gain based on greater daily caloric intake, especially during night (106). The results of a metaanalysis of observational studies, with subgroup analysis by sex, presented that shift work was associated with greater diabetes risk in men (107). Generally, diverse results exist regarding sex and gender differences, referring to the impact of shift work, work stress, and coping (Table 1). Unfavorable effects of testosterone secretion, due to changes of the circadian timing system, were suggested as one explanation. In population-based cohort and occupational cohort studies, job strain overall implicated a higher diabetes risk in women, especially in those perceiving a combination of lack of control and high job demand, as well as low emotional support (100–102). Only 20% of the stress induced diabetes could be attributed to obesity and biological risk factors, thus a mediating effect of employment grade and low SES was suggested. In a population-based study from Germany, men and women with job strain had a 45% higher risk to develop T2DM, independent of traditional risk factors and without relevant sex differences (117).
Controversial results of sex and gender differences in the work-stress-diabetes risk interrelationship may be explained by differences in the interindividual shift work tolerance, in the selection of the occupational groups and the specific definitions of job strain in studies as well as differences in opportunities for recovering from work stress between men and women. In addition to rotating shift work, the individual chronotype and work related circadian misalignment can modulate the diabetes risk in the workforce, as shown for women by the Nurses Health Study 2 (103, 104). T2DM incidence increased in early chronotypes with night shift work and parallel duration of shift work exposure, whereas late chronotypes featured the greatest risk, working daytime schedules. A longitudinal cohort study from Brazil confirmed a sex-specific association between night work exposure and T2DM incidence. After adjustment of confounders, including obesity, much stronger and earlier effects in women were shown (105). At Korean population level, the evening chronotype was more common in younger women and linked to metabolic diseases with sex dimorphism, independent of lifestyle and sleep duration in subgroup analysis. It related to a 3-fold higher risk of T2DM in men and to a 2-fold higher risk of MetS in women (108). Additionally, late chronotype was associated with lower lean mass in males as opposed to females who demonstrated a higher (visceral) fat mass. Another study found that circadian misalignment increased insulin resistance, diabetes risk, and inflammatory parameters, independent of sleep loss with significant sex-by-group interaction. However, the study was underpowered for additional analysis of sex differences (118). Overall, these studies suggest that misalignment between the circadian clock and social rhythms and between sex-dependent biological factors such as body composition and gender-dependent social timing impact pathogenesis of diabetes in men and women.
However, more prospective longitudinal studies are needed to further study these complex sex-dimorphic associations between sleep, work stress, and diabetes. These could help to implement sex-specific prevention programs in specific groups of (shift) workers.
IV. Health Behavior
A. Lifestyle
There are consistent sex differences in health behavior, nutrition, and physical activity, closely associated with risk of T2DM. According to health survey research data stratified by sex, women are overall more inactive but put more effort in healthy nutrition by consuming more fruits and vegetables and less meat (119–122). A prospective, but possibly underpowered, cohort study testing a priori for sex interactions states that women tend to consume more sugar, although high glycemic index diets seem to increase abdominal fat, particularly in sedentary women in contrast to sedentary men (123, 124). In a metaanalysis including predominantly women from observational studies, high glycemic index diets related to increased risk of T2DM (124). As derived from British household surveys, the density of fast food outlets associated with body weight more strongly among women possibly reflecting their greater responsibility in the family setting or maybe lower control of appetite; thus, hinting at a stronger association between body weight and environmental factors. However, the availability of low-priced meals was associated with obesity in both sexes (125).
B. Sugar-sweetened beverages (SSBs)
The rapid economic development and the simultaneously rising consumption of fast food provokes a higher consumption of SSBs, which contributes to the epidemic of T2DM independent of adiposity. In a metaanalysis of prospective cohort studies, men and women consuming SSBs in the highest quantile had 26% excess risk of developing T2DM compared with those in the lowest quantile (126). Half of the effects could be mediated by weight gain in women. Large female and male cohorts evidenced a gene-environmental interaction showing that greater consumption of SSBs is linked to higher genetic predisposition to obesity risk in both sexes (127). In addition, a relationship was found between consumption of more than 2 drinks per day with incident coronary heart disease (CHD) (35% greater risk) in women, followed up for 24 years (128). In a prospective cohort study with separate analysis for men and women, only women showed an increased risk of incident T2DM over 10 years, with a doubled risk seen in women with daily consumption of soft drinks compared with nonconsumers (129). By sex pooling data from national dietary surveys, the model-estimated global burden of diabetes associated with SSB consumption in 2010 revealed 133 000 deaths per year from diabetes and 4.5% of diabetes-related disability-adjusted life years with small differences between men and women. Generally, only a slightly higher number of deaths, however, a minimally lower proportion of deaths attributable to SSBs, was found for diabetes in women compared with men (130). However, there were large regional differences, with high mortality, related to SSB consumption in elder men in Latin America and the Caribbean. Low mortality was observed in younger women in Western Europe and Australia.
C. Alcohol
Moderate alcohol consumption was shown to be associated with a lower risk of T2DM in several observational studies. A systematic review and dose-response metaanalysis of observational studies indicated that relative to current nondrinkers and never drinkers, risk reduction was found in all levels of alcohol intake below 63 g/d with increasing risk above that threshold revealing a significant sex interaction (131). Sex- and ethnicity-stratified analysis demonstrated that risk reduction was specific to women only and non-Asian population. A possible explanation for the sex dimorphism could be that men more frequently have worse drinking behavior with heavy episodic drinking or that alcohol exerts sex-dimorphic effects on glucose metabolism. Indeed, another metaanalysis based on intervention studies showed that moderate alcohol consumption improved glycated haemoglobin in both sexes but tended to improve insulin sensitivity in women only (132). Cross-sectional analysis from the Nurses Health Study indicated that frequent alcohol intake is independently related to higher endogenous estradiol levels and that estradiol alone, or combined with SHBG, influenced the protective association between alcohol consumption and diabetes risk in postmenopausal women (133). Further research is warranted to clarify sex-specific dose-response relationships between alcohol drinking and T2DM risk and the exact underlying mechanisms.
D. Smoking
On the basis of a metaanalysis of cohort studies with subgroup analysis by sex, both active and passive smoking is related to higher risk of developing T2DM in both men and women without known prominent sex differences (134). In a prospective European case-cohort study stratified by sex, overall effects tended to be slightly stronger in men compared with women, although adjustment for confounding factors like obesity, physical activity, or educational level attenuated the association in men but strengthened it in women (135). Based on a sex-specific analysis of a recent metaanalysis, it was estimated that if the association was causal 11.7% of T2DM cases in men and 2.4% in women were attributable to current smoking worldwide (136). However, smoking behavior substantially changed between men and women. In the past decade, it particularly increased in young women, potentially contributing to higher smoking-related diabetes incidence in females in the future (137). In addition, a recent metaanalysis showed that the relative risk of myocardial infarction (MI), an important and frequent complication in diabetic subjects, conferred by smoking appears to be 25% higher in women than in men (138).
V. Pathophysiological Mechanisms With Sexual Dimorphism
A. Developmental origins of health and disease
In the vulnerable phase of pregnancy, many environmental factors have strong influence on fetal development in a sex-specific way (139). Plenty of conditions occurring in pregnancy, such as over- or undernutrition, hyperglycemia, and acute stress situations, for example, are known to influence the phenotype of the progeny via epigenetic effects without affecting the genetic coding directly (140). These epigenetic changes involve DNA methylation, histone modifications, or micro-RNAs. They have the potential to activate or inactivate genes and their subsequent products in manifold ways and can even modify evolution of future generations in a transgenerational and sex-specific mode (140, 141).
B. Fetal programming/epigenetics in animals
Studies on epigenetic effects on diabetes risk in humans are scarce; thus, we mostly rely on studies on rodents. There is evidence that sex-specific intragenerational transmission of glucose tolerance and fat distribution, from one generation to subsequent ones, is caused by maternal undernutrition or hyperglycemia in an epigenetic manner (Table 2) (142–144). In mice, IGT was transferred through both parental lineages, whereas obesity only advances through the maternal line. Reduction in birth weight only appears in transmission through the paternal lineage from F1 to F2 generation (142). In contrast, in another study, a substantial increase of birth weight in F2 was found through impaired glucose tolerant paternal lines (143). Nonetheless, both mothers and fathers transfer an increased danger for IGT to F2 generations, which is especially pronounced through paternal lines (Table 2) (143). Maternal high-fat diet (HFD) in mice was reported to cause sex differences in glucose metabolism in offspring (145). Male offspring in the HFD group had increased oxidative stress, decreased insulin secretion, islet area, and insulin content compared with female mice. Female mice, with mothers on controlled diets demonstrated lower estradiol levels compared with male offspring. The authors pointed out that the sex difference may be explained by higher oxidative stress in male β-cells, which related to decreased estradiol levels, potentially leading to a loss of protection of the β-cells.
Table 2.
Sex Dimorphism in Epigenetic Effects and Genetic Predisposition of Diabetes
| Chr. | Reported Sex Differences | Reference | |
|---|---|---|---|
| Epigenetic effects | |||
| Igf2 and H19 | 2 and 11 | Down-regulation of genes in islets of F1 and F2 offspring of GDM mice caused by altered methylation of these genes (changes of Igf2 and H19 gene expression reported in semen of male F1 offspring of GDM mice); IGT occurs more often in male than in female offspring; in male offspring of low protein-fed rats, higher insulin resistance and lipid levels are reported | 143 |
| G6PC | 17 | Differences in histone methylation and acetylation, hypomethylation of G6PC promoter in male and up-regulated micro-RNAs in female offspring, which results in decreased glucose concentrations and increased enzyme activity of G6PC in male compared with female F1 offspring of low protein-fed sow | 144 |
| IGF2R | 6 | Higher DNA methylation in male offspring exposed to malnutrition | 155 |
| LEP, IL10, APOC1 | 7, 1, 19 | Lower DNA methylation in male offspring exposed to malnutrition | |
| LEP and INS-IGF2 | 7 and 11 | Only in men significant association of malnutrition with DNA methylation | |
| GNAS-AS1 | 20 | In both sexes significant association but higher effect in women | |
| Genetic effects (nearby genes [polymorphism]) | |||
| IRS1 (rs2943641) | 2 | T allele associated with decreased risk of T2DM in women with lower carbohydrate and higher fat intake and in men with lower fat and higher carbohydrate intake | 157 |
| DRD2/ANKK1 (rs1800497, TaqIA) | 11 | Increased risk for T2DM in women but not in men | 193 |
| DRD2/ANKK1 (rs6275) | 11 | Increased first-phase glucose-stimulated insulin secretion in women, but not in men | 193 |
| MIF (rs755622, −173G/C) | 22 | C allele associated with increased abdominal obesity, apolipoprotein B levels, and higher risk for development of T2DM in men | 350 |
| FABP2 (rs1799883, Ala54Thr) | 4 | Homozygous Thr54 variant associated with reduced risk of T2DM in women but not in men | 351 |
| FABP2 (promotor haplotype B) | 4 | Reduced risk of T2DM in men but not in women | 352 |
| NPY (rs16139, T1128C, Leu7Pro) | 7 | C allele associated with IGT and T2DM in men but not in women | 353 |
| UCP2 (rs659366, −866G/A) | 11 | AA genotype associated with T2DM in women but not in men | 354 |
| CCDC63 (rs11065756) | 12 | Associated with T2DM in men, as well as fasting plasma glucose and ß cell function but not in women | 355 |
| HECTD4 (rs2074356) | 12 | ||
| DUSP9 (rs5945326) | X | Association with T2DM | 192 |
| SCARB1 (rs9919713) | 12 | Associates with insulin resistance especially in women | 356 |
| PPARG (rs1801282, Pro12Ala) | 3 | Associated with higher leptin levels in women with T2DM compared with nondiabetic women | 357 |
| Pro/Ala and Ala/Ala allele associated with higher total cholesterol and LDL-cholesterol levels in men with T2DM compared with wild-type allele (Pro/Pro) in men but not in women | 358 | ||
| CNDP1 (5-leucine repeat (5L-5L)) | 18 | Lower cardiovascular mortality in men compared with women | 359 |
| HMOX1 (rs2071746, T(−413)A) | 22 | TT genotype is associated with albuminuria in T2DM; male carriers are at higher risk for albuminuria, not female carriers | 360 |
| ACE (I/D) | 17 | Higher risk for advancement of diabetic nephropathy in T2DM women, not in diabetic men | 331 |
Chr., chromosome.
Earlier studies in overfed mice in gestation and lactation periods demonstrated IGT in male and female offspring of obese mice. Similar differences were shown with lower pancreatic insulin content in male offspring of obese dams (146). Furthermore, in the obese descendant group insulin levels were higher than in the control animal group, independent of sex.
Most recently high susceptibility to obesity and diabetes was demonstrated in a sex- and parent of origin- specific mode in murine progeny (147). Sperm and oocytes of HFD mice were isolated and transferred into healthy foster mothers. In F1 generation, female offspring of HFD parents showed higher adiposity, with nearly similar effects of maternal and paternal gametes. Both male and female F1 offspring exhibited insulin resistance and higher glucose, inherited predominantly through maternal gametes (147).
Maternal HFD plus high sucrose but without obesity during pregnancy exerted sexual dimorphic effects on the regulation of the hypothalamic transcriptome of the offspring (148), showing higher female vulnerability to metabolic disturbances (148). Female maternal HFD offspring presented lower insulin sensitivity and fasting hyperglycemia compared with controlled littermates after birth (148). In males, paraventricular hypothalamic gene expression was down-regulated, potentially indicating an important adaptation to maintain glucose homeostasis in male offspring (148). Additionally, after insulin-induced hypoglycemia, Crh mRNA expression was up-regulated in female offspring only, also demonstrating sexual dimorphism in stress response (148).
Fetal programming was shown to influence hypothalamic neurocircuit formation through central insulin signaling (149). Furthermore, effects of maternal HFD during lactation was recently reported causing obesity and IGT in the offspring through impairment of proopiomelanocortin (POMC) and agouti-related peptide neurons projections to hypothalamic target areas (150). Central hypothalamic insulin signaling interfered with negative feedback to the hypothalamus-pituitary-adrenal (HPA) axis in stressed male mice (151), which potentially explains high comorbidity rates of mental and metabolic disorders (see section V.P). However, sex-specific differences are not yet well documented and need further investigation.
C. Fetal programming/epigenetics in humans
Human males and females born in times of low nutritional resources (famines) are more vulnerable regarding diabetes risk in adulthood with greater risk seen in men. This was experienced for 2 of 3 famines in Austria, which was in between and after the 2 world wars (152). Thus, even in humans, male offspring appear to be more vulnerable in intrauterine life and early postnatal period. However, other studies did not specify any sexual dimorphisms after perinatal undernutrition. Additionally, increased postprandial glucose levels, as well as hyperinsulinemia, were detected in adults affected by food limitation during their pregnancies (153, 154). During Dutch famine, sex-dimorphic alterations of epigenetic profiles were seen in offspring exposed to malnutrition (Table 2) (155). Such variations may explain sex differences in fetal development, at birth, and in later life. Furthermore, the Dutch famine study population showed higher BMI and dyslipidemia only in women, which were exposed to food limitation (156). Further nutrition-dependent sex dimorphisms are detailed in Table 2 (157).
A Scottish human population with and without diabetes, reported a high degree of variation between female and male first generation offspring throughout transgenerational transmission of unfavorable cardiometabolic traits (158). Female offspring, whose mothers had diabetes, were more often affected by MetS, higher glucose levels, and body fat content, rather than female offspring of fathers with diabetes, or no parent diseased at all. Furthermore, lower high-density lipoprotein (HDL)-cholesterol was seen in female offspring, if both parents were affected with diabetes. Both sexes had higher blood pressure (BP), when the mother had diabetes as opposed to the fathers. However, all offspring of diabetic parents have higher risk of increased waist, BMI, and body fat content compared with offspring of parents with no diabetes history. In the light of these sex differences, conveyed by parental T2DM, it is no surprise that predictors of MetS differ in a sex-specific way as well. The most eminent predictors in females were diabetic mother, BMI, and age, whereas in males, they were BMI and body fat. A Japanese study revealed that the body weight of the offspring and parental history of T2DM are determinants of future risk of T2DM in offspring, in a sex-specific way (159). Maternal history of T2DM was related to higher T2DM risk in normal-weight subjects, and history of T2DM in the father was associated with higher T2DM risk in overweight subjects, without showing impact of sex of the offspring.
Regarding smoking, fetal exposure to parental smoking associated independently with risk of T2DM in adult daughters only (160).
D. Fetal sex and risk for GDM
Recently, fetal sex was found to be relevant in pregnancies, for defining the risk of developing GDM and subsequent risk of developing T2DM after pregnancy (89–91). Women carrying a boy in their first pregnancy have a 3%–4% higher risk of GDM and a 7% higher risk when carrying a boy in their second pregnancy. Carrying a girl implies to maintain normal glucose tolerance (NGT) in the first pregnancy. Interestingly, women having GDM in the first pregnancy had 6%–7% higher risk developing T2DM over a median follow-up time of 5 years when carrying a girl (90, 91). In a previous study, it was found that compared with women carrying a female fetus, women with a male fetus had decreased β-cell capacity and higher postprandial glucose levels during glucose challenge (89). Because the underlying mechanism is unclear, the authors speculated different pathophysiological causes for these sex differences in β-cell function in mothers. This might be related to actions of the Y chromosome on sex-specific variations in placenta-derived hormones, because placental lactogen and prolactin or other proteins are involved in β-cell mass expansion (89). Interestingly, especially the placenta shows many sex-specific alterations, also in regard to epigenetic mechanisms, which might truly have huge impact on complications in and after pregnancy. These were recently reviewed in detail elsewhere (161, 162). Moreover, the hypothesis behind higher risk of T2DM in women, after carrying a girl in a GDM pregnancy, could include already existing poorer β-cell capacity of these mothers compared with mothers with a male fetus. The male fetus causes a decrease in β-cell function only in pregnancy, which resolves after delivery and restitutes former capacity. This theory was not proven against actual measures of β-cell function and thus remains speculative. However, it seems that GDM mothers with female fetus have lower β-cell capacity, which lead to higher risk of T2DM and earlier onset over time.
In a secondary analysis, another research group demonstrated that women carrying a female fetus were less insulin resistant when fasting in an early stage of pregnancy but not in a late one (163). As shown in a few previous studies, female newborns had higher insulin resistance compared with male offspring. Interestingly, an earlier study speculated that the usual lower birth weight in girls, compared with boys, might be due to higher insulin resistance in female fetuses during pregnancy. The female fetus does not react to insulin and its trophic actions in the same way as the male fetus does (164). Based on studies reporting higher insulin resistance throughout childhood in females, the authors concluded a genetic background of their Gender Insulin Hypothesis. So far, explanations for these differences are elusive; however, we are now aware of already existing sex-specific differences at the very beginning of life and potentially responsible for many differences in health and disease, in men and women later on. Altogether, these new results highlight the impact of fetal sex on maternal glucose metabolism. The constant interaction between fetus and mother, with potential future negative impact affecting the health of both, clearly demonstrates a health determinant neglect not only in the field of glucose metabolism but also in the field of GDM and fetal sex.
E. Neonatal fat distribution
Already at birth females have more SAT and a more centralized pattern of SAT, assessed by skinfold thickness (165). Remarkably, sex-specific differences in SAT accumulation of neonates were related to their insulin levels (166). The associations between cord blood insulin and different SAT locations were more pronounced in areas typically described as preferential fat storage location, specific for each sex. Overall, these associations were higher in male neonates. Among the 15 measured body sites, neck and upper abdomen were mostly affected by insulin levels. In female neonates instead, this association was only observed with SAT thickness on the hip. Based on these observations, sex-specific body shape and lipid accumulation could already be determined in utero, especially in insulin sensitive locations varying by fetal sex. Furthermore, these observed differences in SAT might be allegeable with smaller insulin effects on SAT, due to above described higher insulin resistance in female neonates.
F. Small or large for gestational age neonates
Birthweights under and over the normal limits are associated with metabolic disease as reported throughout literature (167). Sex differences were found in several studies with controversial results, regarding the risk of T2DM for subjects born with low birth weight (LBW) or high birth weight. In a recent Swedish register study (168) investigating nearly 760 000 individuals, high birth weight was related to increased risk of T2DM and obesity. Males already had a higher risk for T2DM in lower weight categories, among high birth weight group. This risk was exaggerated in the highest birth weight categories in men compared with women. In a Danish register, with more than 220 000 men and women, LBW and high birth weight were reported to result in a higher risk for development of T2DM in women (169). Women in the high birth weight group had a higher risk for T2DM compared with men. In the LBW group, only women were affected by the higher T2DM risk. A small observational study found the opposite in very LBW offspring, with male sex being an independent risk factor for hyperglycemia (170). In this study, men with very LBW had higher levels of glucose, lower levels of insulin and reduced β-cell function compared with women with comparable insulin resistance.
These studies demonstrate a strong relation of birth weight and T2DM risk in both sex cohorts. Register studies revealed associations of LBW and T2DM in women and a higher risk for men categorized as large for gestational age (168, 169). Nonetheless, studies are controversial and further research is needed to fully understand sex-specific associations of LBW and high birth weight with glucose metabolism.
Additionally, both over- and undernutrition as well as hyperglycemia in pregnancy are associated with increased risk for cardiorenal disease in the offspring. Especially in this vulnerable phase, the kidney is prone to a number of mechanistic changes driven by epigenetic alterations. These can lead to renal dysfunction, glomerular hypertrophy, diminished vasodilative renal vessel function, changes in renin-angiotensin system expression followed by hypertension in adult life, usually more often affecting men. These aspects were summarized in a recent review, also highlighting sex dimorphism in kidney disease (171).
A study reporting on induced fetal lung maturation, using glucocorticoid bethamethasone, identified increased insulin concentrations in adult female offspring only (172). A higher reactivity of HPA axis, after prenatally prescribed glucocorticoids, was reported in female offspring between 6 and 11 years of age (173). Therefore, higher sensitivity of HPA axis may already exist in this very early period of life in female offspring. A more responsive HPA axis was also described in elder women compared with men (174). However, in both sexes, higher HPA axis activity was clearly related to lower birth weights with no sex difference (174). These results confirmed previous findings in animal studies, which showed higher HPA reactivity in female offspring after exposure to glucocorticoids or stress in the mother (175, 176). Interestingly, excess HPA axis reactivity was identified in some studies to be involved in pathogenesis of psychiatric disorders, as depression, as well as cardiometabolic disease (177, 178). Further studies are needed to clarify the relationship between birth weight, pregnancy-related stress and HPA axis activity of offspring and the impact of programming adult diseases in young men and women.
G. Endocrine disruptors
Exposure to endocrine disruptors is supposed to contribute to higher risk of obesity and T2DM in humans (179). A dose-dependent positive relationship was noticed between urinary phthalate metabolites and parameters of glucose metabolism (fasting glucose and insulin resistance) in both sexes (180). However, pathophysiological mechanisms behind disrupting actions are mostly based on surrogate markers and not well understood at the moment. Endocrine disruptors are already able to act as hormones in low but persistent dosages, mostly mimicking estrogen properties. They either activate or inactivate cellular receptors, cell responses, and other targets and can cause higher insulin resistance and hyperinsulinemia. Furthermore, persistent exposure to small dosages appears to be related to mitochondrial dysfunction due to intracellular gluthathione depletion. This associates to inflammation and ectopic fat, potentially leading to T2DM. Candidate obesogens cover a wide range of compounds, including bisphenol A (BPA) and phthalates (179). Endocrine disruptors mostly travel with lipids and accumulate in adipocytes causing reactive changes in adipokine levels, which happen in a sex- and disruptor-specific way.
In the Canadian Maternal-Infant Research on Environmental Chemicals Study, newborns showed significant sex differences in leptin and adiponectin levels, which were associated to maternal in utero BPA exposures (181). Female offspring had higher leptin levels than males, whereas adiponectin did not differ but was inversely related to BPA in males. On the other hand, high leptin levels in males were especially seen in moderate to high exposure when compared with mono-(3-carboxypropyl). In another study investigating mother-child pairs, late in utero BPA exposure related to increased plasma leptin levels in boys, whereas early exposure was linked to higher plasma adiponectin in girls at the age of 9 years (182). Sex differences in key metabolism-related hormones, referring to BPA and phthalate exposures in utero and childhood, were corroborated by another study showing additional results regarding exposure time and differentiating by pubertal status next to sex in adolescent offspring (183). In utero monoethyl phthalate was associated with higher leptin levels in girls and decreased insulin secretion in pubescent boys. Monobenzyl phthalates related to lower leptin levels in girls only. This study also investigated peripubertal BPA and phthalate exposure, which was related to higher leptin in boys. The combination of mono-n-butyl-phthalates and monoisobutyl phthalates associated with C-peptids in boys. In addition, only pubertal boys had lower IGF-1 concentrations, which were also related to various urinary phthalate metabolites. In girls, another compound, di-2-ethylhexyl phthalate, was associated with increased IGF-1 levels in prepuberty. Pubertal girls were affected by higher glucose levels during fasting, which was associated with various phthalate metabolites.
Therefore, overall sex-specific associations between BPA and leptin were found in boys in both studies but with different exposure times and developmental periods (182, 183). These discrepancies are supposed to be caused by different populations either from urban or rural areas with varying BPA exposures. Although underlying mechanisms of endocrine disruption through chemicals in humans are still unclear, the peroxisome proliferator-activated receptors (PPARs) and reactive oxygen species are yet suspected to play a major role (183). In animal models, PPAR expression is altered through endocrine disruptors, and thus subsequent alterations in metabolic parameters result. Of note, PPAR expression is sex-dependent (184). Hence, if endocrine disruptors have the potential to change metabolism in humans via alterations in PPAR expression, sex-specific differences will have a causal explanation.
Further studies need to give wider insight into the uncharted interactions of genes and environment in animals and humans. Considering their transfer and phenotypic transmission throughout the offspring generations. At present, in human surveys, the underlying mechanisms are limited and sex-specific investigations are urgently needed for epigenetic effects on limited nutrient supplies, as well as food overload, environmental factors, and hyperglycemia.
H. Genetic predisposition
Even autosomes display divergent expression patterns in gene regulation either mediated through hormones or directly modulated by sex chromosomes. Sexually dimorphic gene expression across organs vary, between 14% in brain and 70% in liver, with mostly small effects (185). Additionally, sex differences were recently also described in the transcriptome of human placental cells, demonstrating an influence of fetal sex on placental gene expression in a cell-type dependent manner (186). Thus, placental function appears to be affected differently for male or female offspring, potentially framing sex differences in metabolic, immunological, and inflammatory responses (186). In a recent study presenting genome-wide association metaanalysis, the genetic background of body fat accumulation and its relation with cardiometabolic traits was investigated (187). Sex-specific differences were found in 20 out of 49 genetic loci, which are involved in regulatory functions of adipose and insulin biology. According to the waist to hip ratio, stronger effects were seen in women in almost all associations of these loci. In particular, these associations were related to higher WCRs in women and to lower hip circumferences in men.
Next generation sequencing in obese diabetic ZSF1 rats, featuring a model of T2DM, revealed 103 genes showing sex differences in genes expressed in the liver (188). Genes involved in lipid metabolism and glycolysis were associated with female-specific genes, whereas hepatic metabolism, detoxification, and secretion were associated with male-specific genes. These results suggest a huge variety of genes showing sex dimorphism in hepatic genes, which might influence drug pharmacokinetics in a sex-specific way. This calls for a further urgent clarification of its impact on clinical outcome in humans.
Another way of looking at genome-wide association study results is the so called pathway-based approach, which links SNPs considered mutually involved in a pathway. This multilevel approach might give further understanding of mechanism behind genes and their relevance in diseases. Heterogeneity between males and females was identified in gene sets associated with T2DM in humans (189), 5 pathways were identified in the male group and 13 in the female group, with only 3 pathways overlapping. In the male group, the gene TCFL7L2 largely contributes to the significance of these pathways, whereas in women, no such effect was reported.
I. Gonosomes
The number of X chromosomes within cells contributes to sex differences in adiposity (190). Accelerated weight gain on HFD, incident hepatic steatosis, and hyperinsulinemia of XX animals mainly depended on the amount the X chromosomes. Higher expression of a subset of genes on the X chromosome, which escaped inactivation, is seen in adipose and liver tissue of XX animals compared with XY animals (female cellular mosaicism). GH expression might be stimulated through the number of X chromosomes and X inactivation and is involved in impaired energy metabolism (191). Furthermore, one locus near dual specificity phosphatase 9 on the X chromosome is directly associated with higher T2DM risk (192).
A couple of sex differences in genes associated with T2DM were investigated so far (Table 2). Most of these identified genes, conveying sex differences in diabetes risk, increased in one sex without showing any effect in the other. In some genes, the ability of reducing T2DM risk was observed to differ between men and women as well. Furthermore, differences in leptin, lipid, and glucose metabolism were demonstrated, which are based on genetic sex differences (Table 2). In T2DM, cardiovascular mortality was lower in men compared with women carrying a leucine repeat in carnosinase gene.
Sex-specific differences in the ANKK1 (rs1800497) polymorphism of dopamine receptor D2 in humans were reported with increased risk for T2DM in women, which could not be found in men (193). Furthermore, another polymorphism in women was found to be associated with elevated first-phase insulin secretion (193). However, sex differences in regulatory mechanisms of genes could be the key element in explaining sexual dimorphism, leading to variations in phenotype through gene-environment interactions (194). Although a large number of T2DM risk genes were found so far, the effect size of single risk alleles or the predictive accuracy of combined genetic risk scores of incident T2DM is rather low up to now (195). A small improvement in risk prediction could be achieved by the use of a genetic risk model, even in a sex-specific very high-risk group like women with GDM. The additive value, in addition to traditional anthropometric and metabolic clinical parameters, in prediction of diabetes risk appears to be small. However, one reason among many others could be the heterogeneity of subjects with T2DM next to the polygenetic nature of the disease, missing heritability or that important biological factors including sex, age and ethnicity were neglected in many studies. Sex had a small but significant impact on the genetic T2DM risk model, which disappeared in the combined genetic and lipid metabolites risk model in the Framingham offspring cohort (196). Still, also in this study, genetic markers of diabetes risk only modestly improved the predictive accuracy of future occurrence of T2DM, based only on traditional clinical risk factors. Nevertheless, improved and maybe sex-specific genetic and epigenetic risk models could help to develop personalized medicine in the future.
A comprehensive overview of genes associated with T2DM or involved in metabolic function, relating to complications or mortality featuring sex dimorphism in T2DM so far, are shown in Table 2.
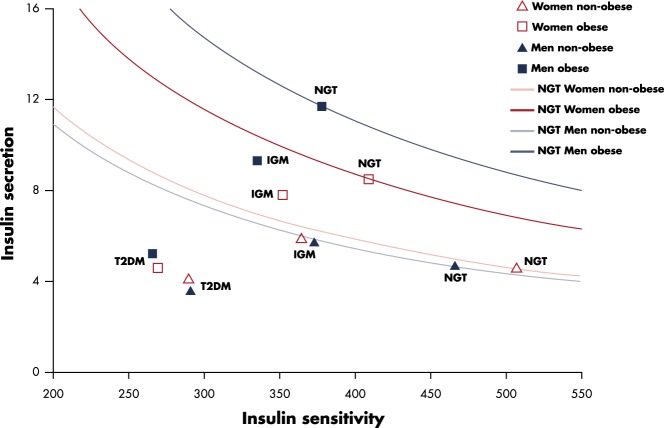
J. Glucose tolerance
IFG is more prevalent in men and IGT more frequent in women, regardless of their ethnicity. These metabolic conditions, together with T2DM, are related to glucose handling by the whole body, which is evaluated by the glycemic levels at fasting and in postprandial conditions. The 2 major processes responsible for the maintenance of normal glucose levels are insulin resistance/sensitivity and insulin secretion. In general, NGT is maintained if increased insulin secretion is able to compensate the reduction of insulin sensitivity, which occurs for instance, with increasing BMI or age (197). Figure 5 shows this phenomenon of the classic hyperbolic paradigm, ie, the nonlinear inverse relationship between the 2 processes. As long as a subject is able to balance the 2 processes, he/she remains on the “normal” curve. When the balance insulin sensitivity/secretion and their interplay fail, because 1 or both deteriorate, the subject moves in the lower part of the graph in the bad “zone,” featuring prediabetes/IGM and eventually reaching a status of overt T2DM (197, 198). We have applied these concept to a large European population to evaluate possible sex differences in the metabolic parameters across various glucose tolerance categories (199).
Figure 5.
Insulin secretion and sensitivity in men and women with NGT, IGM (IGT and/or IFG), and overt T2DM relationships between insulin sensitivity, calculated as oral glucose insulin sensitivity (OGIS) (m−2 mL/min) (367), and insulin secretion, as the AUC of insulin (min U/L), from oral glucose tolerance test (OGTT) data. Continuous lines represent the normal metabolic condition (NGT) in both nonobese and obese males and females, ie, for declining insulin sensitivity, there is an increase of insulin secretion to compensate for insulin resistance, maintaining NGT (200). The location of the various categories of subjects is positioned by the different symbols according to their combination of insulin sensitivity and secretion. In general, the “good” area is that above the curves for the nonobese subjects, whereas the “bad” one is below and especially in the low left corner characterized by low insulin sensitivity and inadequate secretion. Original data derived from different studies carried out by the authors (199, 200).
K. Insulin sensitivity and secretion
Nonobese subjects exhibit glucometabolic sex differences only in the NGT group, where women are more sensitive than men (Figure 5) (200). When glucose tolerance deteriorates toward IGM, insulin sensitivity in women is reduced more than in men. An increased secretion is observed in both sexes, which was enough to maintain the subjects close to the appropriate compensation curve, derived from the normal-weight healthy control subjects. In T2DM, the impairment of insulin sensitivity and insulin secretion is substantial and similar in both sexes. These evidences are confirmed also when introducing age and BMI as covariates into the whole population, ie, insulin sensitivity decreased with increasing BMI at the same rate for both men and women in all glucose tolerance categories, whereas insulin secretion increased with BMI at a faster rate in men, which better compensated the increasing insulin resistance. This trend may partly explain why, in general, women show better insulin sensitivity and overall more favorable cardio-metabolic risk profiles, than males if normoglycemic. This may be associated with sex hormones and their receptors, different body fat distribution and related biomarkers, such as higher adiponectin, which are discussed earlier. Estrogen demonstrated protective effects from β-cell apoptosis (201), stimulates β-cell secretion (202) and improves insulin sensitivity (203) with antidiabetic effects primarily described to ERα (68, 204). Estradiol administration increases insulin-mediated glucose disposal in early postmenopausal women but such benefit is not seen in late postmenopausal women (205).
With age-induced deterioration of glucose tolerance, sex differences are reduced, leading to more pronounced aggravation of the metabolic profile in women than in men (206, 207). This is mediated by greater adiposity and insulin resistance (33). This aggravation, therefore, may be related to the fact that women have to gain more weight to develop T2DM (208). Nonetheless, the rate of onset of T2DM is greater for men than for women in different ethnic groups (209) at lower BMI levels. Another reflection of the above conclusions is the importance of performing, when possible, a “full” test with insulin measurements, for instance, an oral glucose test (210), in order to better characterize the single metabolic parameters in both healthy subjects and patients, especially women.
L. Incretin hormones
Differences in insulin secretion could be partly ascribed to the effect exerted by the incretin hormones during an oral test on pancreatic β-cells. To the best of our knowledge, there is no recent study that thoroughly investigates the role of sex on the incretin effect. In an early review, it has been reported that the magnitude of the effect of glucagon-like peptide-1 (GLP-1) does not greatly depend on patient characteristics, such as age and sex (211). More recently, GLP-1 response was evaluated in a large cohort of subjects of both sexes, with different degrees of BMI and ranging from NGT to T2DM. Women with IGM or T2DM, independently of age or obesity, had 25% lower GLP-1 response to an oral challenge than those with NGT with consequently lower GLP-1 concentration (212). Because higher GLP-1 responses are associated with better insulin secretion, the low incretin levels could partly explain the reduction of β-cell function observed in women when becoming IGM or T2DM.
M. Gastric emptying and glucose absorption
In studies carried out with an oral test, “postprandial” glucose metabolism is influenced by gastric emptying and intestine glucose absorption. Gastric emptying of carbohydrate containing meals has been demonstrated to positively correlate with postprandial glucose levels (213), and it has been studied in healthy control subjects and in diabetic patients. In both cases, gastric emptying was found to be slower in women than in men, although the etiology of this sex difference remains to be clarified (214). Recently, attention has been devoted to gut glucose absorption, because it could contribute to explain why in general women exhibit higher 2-hour glucose levels during an oral test. However, only few studies have been performed. In general, in lean subjects, meal appearance in the peripheral circulation was found higher in women than in men, irrespective of age (215). More recent investigations showed no differences in the amount of absorbed glucose when adjusted for age, height, and/or fat-free mass (212, 216) but only proved a prolonged gut glucose absorption in women, probably due to a slower gastric emptying. These factors could then contribute to higher glycemic levels during the oral test and thus to the evidenced higher prevalence of IGT in women.
N. Ectopic fat
Impaired lipid metabolism with excess release of FA from adipose tissue leads to overspill of circulating lipids and thus to ectopic nonadipose lipid accumulation in the liver hepatocellular lipids (HCL), muscle intramyocellular lipids (IMCL), and myocard myocardial lipids (MYCL) with detrimental consequences of lipotoxicity. Of these facts potential sex differences may emerge (56).
Sex-dimorphic results were seen in IMCL, depending on total body fat content and lifestyle. Among younger normal-weight sedentary volunteers (217) and also in obese and diabetic subjects (218), females had higher IMCL in leg muscle (219), higher lipid area density, and greater number of IMCL droplets than males. Women also tend to oxidize more fat than glucose after endurance exercise training (220). Women presented to have double the amount of IMCL as men and to experience a net reduction in IMCL during prolonged exercise. Women at high risk of T2DM, with previous insulin-treated GDM, showed an IMCL increase of up to 60%, whereas insulin sensitivity and ATP-synthesis were only slightly decreased at that stage (221, 222).
Men more often developed fatty liver disease than females, due to more pronounced insulin resistance, different effects of gonadal hormones and environmental aspects (Figures 2 and 3). Estrogen is protective in both sexes, and estradiol treatment improved insulin resistance and HCL levels in animals (223). Nevertheless, the balance of sex hormones appears important as inappropriate low testosterone, or high estrogen concentrations in males, may also relate to fatty liver disease and metabolic abnormalities. In normotolerant young women, with previous GDM, liver fat was twice as high as in women with normal pregnancy, considering insulin resistance and body fat (222). Also later the manifestation of overt diabetes (224) was predicted.
Increased MYCL is one of the many potential pathophysiologic mechanisms implicated in “diabetic cardiomyopathy” (225). Healthy women have lower MYCL and pericardial fat than men (226). Male sex and glycemia independently predict heart steatosis. Glucose tolerance deteriorates the increase of MYCL, which was more pronounced in women, abrogating sex differences in T2DM. This potentially attenuates cardiac protection in diabetic women. Consistently, MYCL increased in diabetic women, whereas stroke volume decreased and heart rate increased; this was already initiated in insulin-resistant nondiabetic women (227). Also nondiabetic women, with previous GDM, had no cardiac steatosis or dysfunction, although myocardial wall thickness related to glycemia and BP. Thus, increased MYCL does not appear to be an early marker in the pathogenesis of diabetes but a consequence of chronic hyperglycemia (228).
O. Energy imbalance
Sex dimorphism, in substrate and energy partitioning (Figure 3), has been clearly described in details in recent reviews (229, 230). At rest, women have greater storage of free FAs than men, but during exercise and conditions of sustained increased demand, women were shown to exert higher oxidation of lipids in relation to carbohydrates. Males instead rely relatively more on glucose and protein metabolism (Figure 3) (66). During times of food deprivation, females reduce energy expenditure with consequent loss of fat stores contrary to males. This can explain greater harm in males in periods of undernutrition.
Estrogen can decrease food intake directly by effects in the brain. Tight interacting of leptin, insulin, neuropeptide Y (NPY), and ghrelin seem to play a vital role (231). Moreover, estrogen can exert direct effects on fat tissue by enhancing proliferation of preadipocytes, especially in females (232), and by up-regulating sc α2A-adrenergic receptors promoting SAT accumulation, notably in premenopausal women (233). Polymorphisms in the ERα gene were found to relate to increased abdominal fat in young women (234). Both female and male ERαKO mice were shown to develop adiposity, which may be primarily due to reduced energy expenditure (235).
Women display less reduction of insulin sensitivity with increasing body fat and lower resting energy expenditure, which declines more rapidly with ageing compared with men. Menopause is associated with decrease of total energy expenditure due to the loss of estrogen effects on the hypothalamus via increased release of orexigenic hormones NPY, agouti-related peptides, and a decrease in lean body mass (67). In postmenopausal women, the most important source of estrogens is fatty tissue where adrenal androgens are converted into 17β-estradiol and estrone catalyzed by aromatase. A higher conversion rate in obese and/or older women is probably due to the higher number of adipocytes (236). Females may exert a higher capacity for adipocyte enlargement and adipose tissue plasticity may play a role in obesity-related metabolic abnormalities and ectopic fat deposition (237). The sum of all these effects could contribute to the higher rate of the metabolically healthy obese phenotype in women.
Testosterone has shown to inhibit lipoprotein lipase and uptake of triglycerides by adipose tissue (238), to increase lipolysis via β-adrenergic receptors (238), and to promote increase of fat-free mass and muscle insulin sensitivity by increasing mitochondrial capacity (78). It is noteworthy that estrogen deficiency but not testosterone deficiency per se is responsible for the increase in body fat mass in males, but androgen deficiency induced a decrease in lean body mass, muscle size, and strength (239).
Recently, also the composition of gut microbiota has shown to be associated with energy balance, the risk of insulin resistance and diabetes, potentially via changes of the FA metabolism or via release of gut-derived hormones (56). Preliminary results have pointed out potential sex-specific gut signatures related to obesity and diabetes with more unfavorable proinflammatory gut microbiota components in males (240). However, up to now, only very few studies have reported results, stratified by sex. Future research would demand bigger studies to clarify whether sex differences also play a relevant role in microbiome-dependent hormone regulation and microbiome-related metabolic diseases, like T2DM, as shown for type 1 diabetes (241).
P. HPA axis activity and stress model
The hypothalamus regulates food intake and energy homeostasis and coordinates important metabolic and endocrine processes, as well as the autonomous nervous system. Females have higher estrogen-related POMC, an anorexigenic prohormone synthesized by the hypothalamus and pituitary gland, which results in important derivates like ACTH and α-melanocyte-stimulating hormone, which influence appetite and energy expenditure (242). POMC neurons express insulin and leptin receptors. Glucocorticosteroids play an important role in adipogenesis, lipolysis in fatty tissue, and hepatic insulin resistance, potential sex differences regarding basal or stress-induced HPA axis activity have been observed (243). 11β-hydroxysteroid dehydrogenase type 1 converts cortisone in cortisol, thereby increasing local glucocorticoid levels in liver and adipose tissue, particularly in VAT (244). Some studies have shown higher sensitivity to ACTH and cortisol in women and lower ACTH and cortisol levels in younger women including lower circadian variations. However, there was no difference observed between postmenopausal women and men of comparable age (245). Across the cycle, estrogens may increase ACTH release and corticosterone levels, related to estrogen levels, whereas androgens exerted an inhibitory effect on the HPA axis stress response (245). Especially women with abdominal obesity feature increased cortisol release to acute stress challenges. Interestingly, the adrenal response to ACTH was higher in healthy young women as well as in postmenopausal ones, compared with men. However, these sex differences disappeared in patients with overt T2DM (246). Therefore, diabetic men had higher peak cortisol levels compared with controls, but the clinical implications of this finding are so far unclear. Further studies present an association in women between the stress level and the activation of the vascular endothelial nitric oxide (NO) system, as well as with the carotid intima media thickness, suggesting a close link to stress induced cardiovascular dysfunction in women (99).
Insulin resistance/hyperinsulinemia influence neuroendocrine pathways and relate to sex hormone imbalance. HPA axis and sex hormones appear to mutually interact by impairing stress responses, thereby enhancing visceral obesity phenotype and related metabolic abnormalities (111, 247). Acute stress leads to increased glucocorticoid release from the adrenal glands combined with sympathetic arousal, activation of the renin-angiotensin system, release of inflammatory cytokines, and changes of the immune system (247). A vicious cycle is then established: chronic stress results in disturbed energy homeostasis and feeding behavior (248), leading to VAT accumulation and insulin resistance, which is further aggravated by sympathetic overactivity. Testosterone deficiency aggravates the MetS in men by bringing forward obesity and hyperinsulinemia, which in turn suppresses testicular androgen production (“vicious cycle”) (also discussed in II.G). In obese women, androgen excess, related to increased HPA activity, implicates unfavorable cardiometabolic effects.
Ghrelin and the orexigenic anxiolytic NPY increases with stress contributing to “emotional eating,” which appears to play a greater role in females, mediating the stress-obesity-diabetes relationship. Stress potentiates craving for energy-dense food and impacts food reward. Women appear more vulnerable to stress-related weight gain (249). In addition, women were shown to have lower ability to suppress hunger (250). In general, women appear to exert higher HPA sensitivity and therefore tend to be at higher risk, than males, of diseases associated with HPA dysfunction. HPA dysfunction relates to eating pathologies and psychiatric disorders, like major depression and anxiety disorders. These are much more frequently diagnosed in obese or diabetic women than men. Depression may disrupt HPA axis, thereby increasing levels of cortisol, catecholamines and inflammatory cytokines, potentially even in a sex-specific manner (251, 252). Additionally, depression can unfavorably influence lifestyle, dietary intake, and physical activity further aggravating diabetes and obesity. As discussed above, it has been speculated that sleep loss or sleep disturbances, related to rotating shift work, and desynchronized circadian rhythm may induce glucose intolerance by stimulating similar neuroendocrine pathways (113, 253). Interacting circuits of the circadian clock system and metabolic elements involve central pacemaker neurons of the suprachiasmatic nucleus regulating sleep-wake cycle, feeding schedule and behavioral rhythm. Besides the peripheral clocks at the level of liver, muscle, fat, and pancreas are also regulated (254). A possible link between circadian clocks, regulation of glucose metabolism, and melatonin signaling in the pancreas was indicated by genetic studies (255). Melatonin is a hormone that causes chronobiotic peaking at midnight. Reduction of its release during shift work appears to contribute to deterioration of insulin resistance and glucose intolerance (256). Furthermore, lower melatonin levels were described in depressed patients and were found in elder women compared with elder men, independent of light exposure (257). Additionally, circadian misalignment is associated with alterations in cortisol and leptin secretion in relation to wake-sleep and feeding-fasting cycles causing further aggravating dysregulation of glucose and energy homeostasis (258, 259).
Q. Hypothalamic melanocortin system
Sex-different behavior is influenced by a sex-dimorphic hypothalamic melanocortin system (66, 260). POMC peptides are involved in the regulation of energy and glucose metabolism. Male mice showed decreased anorexigenic neuropeptide POMC genes and protein expression, which related to increased energy intake (260). In these POMC neurons, leptin receptors in the hypothalamic arcuate nucleus display important sexual differences (261). Glucose metabolism is influenced to a greater extent by leptin receptors in POMC in males, whereas lipid distribution is more intensely influenced in females (261). Furthermore, female rats were more sensitive to the anorectic effects of centrally injected leptin rather than male rats, which on the contrary were more sensitive to centrally injected insulin (262, 263). After ovariectomy, female rats exhibited higher central insulin and lower leptin sensitivity, which could be restored by estrogen administration (262). Therefore, the mechanism proposed behind decreased female central insulin sensitivity is a modulation caused by brain estrogen signaling, potentially mediated by estrogen effects on ERα in various regions of the hypothalamus. These effects are also centrally involved in the regulation of body weight. Interestingly, estrogen effects within the brain with consequent alterations of leptin and insulin sensitivity could also be verified in male animals after estrogen administration (262). This is in agreement with findings in juvenile male and female rats with low levels of gonadal hormones. These featured similar anorexigenic effects of intranasal insulin with decrease in meal frequency and total food intake together with comparable changes in hypothalamic gene expression (262, 264). These anorexigenic central nervous insulin effects shall be interesting for potential therapeutic approaches to treat childhood obesity in both sexes.
Central insulin action is impaired by binge drinking to a similar extent in male and female rats (265). This may be potentially caused by decreased insulin receptor and protein kinase B phosphorylation in the hypothalamus, such as increased inflammation and expression of down-regulating elements of the insulin signaling cascade (265). Glucose tolerance was more disrupted in female rats after binge drinking than in male rats. The authors demonstrated that hepatic and adipose insulin effects were disturbed as a secondary effect to hypothalamic insulin resistance (265). Moreover, it was found that the inactivation of the brain insulin receptor caused increased food intake in female mice (266). However, both sexes showed an increase of body fat, insulin resistance, leptin, and triglyceride levels as well as impaired reproduction (266).
In genetically programed insulin-resistant obese mice with increased appetite and reduced physical activity, targeted restoration of Pomc function only within 5- hydroxytryptamine 2c receptor containing cells induces sex differences in energy balance (267). Although food intake and insulin sensitivity improved in both sexes, female mice remained physically inactive with low total energy expenditure and higher fat mass (267). This may also have implications for antiobesity treatment in humans, because new drugs target these key regulators of energy balance, restoring impaired POMC neuron function.
Fundamental sex differences in central insulin signaling were corroborated in humans (16, 262, 267, 268). Also in humans, both insulin and leptin play important roles in regulation of energy metabolism and body weight via central and peripheral effects. Intranasal insulin decreased fat mass and reduced feelings of hunger and leptin levels in men only, confirming higher sensitivity to catabolic insulin action of male brains (16, 262, 269). Additionally, intranasal insulin application suppressed systemic lipolysis and reduced circulating free FA concentrations in healthy men and women, independent of blood insulin or leptin concentrations, presumably mediated by central nervous system insulin signaling (268).
Based on all these studies, new treatment options may be available in future, which target the central regulation of energy metabolism and glucose homeostasis. Translating these evidences into human terms, elicits that consideration of possible sexual dimorphism is compulsory. Generally, more studies in humans are currently needed regarding this important field of research.
VI. Cardiovascular Complications
A. Risk factors
Table 3 gives an overview of sex differences regarding major diabetic complications and frequent comorbidities. It is hypothesized that diabetes attenuates the general female biological advantage by protecting against cardiovascular complications across all ages (206, 207). Reproductive factors, differences in experience, and presentation of symptoms or psychosocial stress may also play a role in the more unfavorable situation of diabetic women. Additionally, comorbidities, including depression, greater “cardiometabolic load,” and inflammation, are already present in an early phase of T2DM, as well as later diagnosis in women probably contributes to persisting discrepancies in cardiovascular complications between men and women. A global study showed that there were sex differences among various risk factors for MI; besides diabetes, also hypertension, low physical activity, and high alcohol intake were stronger predictors for MI in women rather than in men (270).
Table 3.
Sex-Specific Differences in Complications and Comorbidities of Diabetes
| Parameter | Men With Diabetes | Women With Diabetes | Notes | Reference |
|---|---|---|---|---|
| Comorbidities | + | ++ | Overall, higher burden in women | 335, 361 |
| Physical limitations | + | ++ | More physical limitations in women than men (60% vs 54%) | 335, 336 |
| Cognitive limitations/geriatric conditions | + | ++ | More cognitive limitations in women than men (19%–34% vs 7%–21%) | 335, 337 |
| Higher risk of cognitive impairment, depression, and falls in women | ||||
| Depression | + | ++ | Higher prevalence of depression in diabetic women than men (10%–33% vs 8%–14%) Stronger association between diabetes and depression in men |
335–337, 339, 340, 362–364 |
| Anxiety | + | ++ | Higher prevalence of anxiety in diabetic women than men (20% vs 11%) | 340, 363 |
| Pregnancy complications (women with GDM or T2DM) | n.a. | + | Higher risk for primary cesarean section, preeclampsia, premature delivery, stillbirth, and perinatal mortality Diabetic embryopathy (abortus, congenital anomalies), diabetic fetopathy (macrosomia, birth weight, and body fat >90th percentile, fetal hyperinsulinemia) |
87, 365 |
| Sexual dysfunction | + | + | 25%–50% mild to severe erectile dysfunction (ED), 50% female sexual dysfunctions | 76, 342–345 |
| ED may serve as marker of risk of future CVD | ||||
| Nephropathy | + (+) | + (+) | Faster progression of diabetic nephropathy in men More males on dialysis therapy and with kidney transplantations |
318, 321, 330 |
| Higher risk of proteinuria and renal disease in women than men among T2DM subjects | ||||
| Lower extremity amputations | ++ | + | Men: more likely to develop foot ulcerations, peripheral vascular disease and neuropathy, shorter long-term diabetic foot patient survival | 312, 317 |
| Women: higher mortality related to amputations | ||||
| CHD | + | ++ | Diabetic women bear a 40% greater relative risk of CHD compared with male counterparts; greater risk for both fatal and nonfatal events | 270, 274 |
| Stroke | + | ++ | Diabetic women experience a 27% greater relative risk of stroke compared with men; greater risk for both fatal and nonfatal events | 273 |
| Mortality | + | ++ | More years of life lost at age of 40 in diabetic women than men | |
| Morbid obesity | ++ | + | Two-fold excess mortality compared with lean subjects, with greater reductions in life expectancy in men; age-adjusted cause-specific mortality rates showed greater increase caused by heart disease and diabetes in men but by cancer in women | 298, 366 |
| Vascular | + | ++ | Although in absolute numbers more deaths occurred in diabetic males than females, compared with nondiabetic subjects, risk was particularly higher in younger subjects and among women | |
| On dialysis | + | ++ | Men present more CVD comorbidity | 319–322 |
| Excess mortality in diabetic women on dialysis | ||||
| Higher mortality risk after first renal replacement therapy in women than men with T2DM |
+, increases risk; ++, increases risk to a greater extent.
B. Coronary heart disease
In newly diagnosed diabetic subjects without clinical CVD, increased atherosclerosis and higher intima media thickness was found in carotid arteries (271). In general, male sex, besides age, was stronger associated with carotid plaques than female sex. However, subgroup analysis revealed that as opposed to male groups, carotid atherosclerosis was more prevalent in newly diagnosed diabetic women than in nondiabetic female controls. This data confirms that diabetes, even at an early stage, attenuates the protective effect of female sex and increases the risk for CVD in females to a greater extent than in males.
The presence of MetS and visceral adiposity predicted development of CVD largely independent of diabetes in men but primarily via IGM in women (272). Diabetes is also a greater risk factor for nonfatal incident CVD in women than men (273, 274). The cause of this excess risk of diabetic women is still not completely understood, but many biological and environmental factors play a role. Physiologically speaking female sex hormones have beneficial effects on cardiovascular wall properties, which are reviewed in detail elsewhere (275, 276). However, diabetes impairs endothelial response in women more dramatically than in males modifying the beneficial hemodynamic estrogen effects by complex interactions between insulin and estrogen signaling. Hyperglycemia adversely modifies the balance of expression and activity of ERs (277). Also, an increase in oxidative stress and endothelin-1 can be observed. This further promotes vasoconstriction and platelet aggregation (278) and decreases endothelium-dependent relaxation and NO production via impaired insulin signaling (277). In diabetic rat models, female mesenteric arteries show greater abnormal vascular responses demonstrated by greater impairment of acetycholin-induced relaxation and an increased expression of endothelial nitric oxide synthase. Thus, a relative reduction of endothelium-derived relaxing factors with greater reliance on NO can be expressed. These modulations of vascular reactivity in diabetic animals may predispose female arteries to vascular injury (279).
Hyperglycemia inhibits antiproliferative effects of estrogen on vascular smooth muscle cells. These are mediated through selective ERα activation under normoglycemic conditions. Hence, beneficial effects are counterbalanced by simultaneous ERβ activation, leading to loss of protective estrogen effects (280). This causes a proinflammatory environment accelerating atherosclerotic processes and CVD particularly in diabetic women. However, this might also serve as a potential therapeutic pathway. In addition, mutations of ERα relate to insulin resistance and early atherosclerosis in young males (281, 282).
An indisputable effect of sex hormones on endothelin-1 expression was reported in humans with androgens increasing and estrogens decreasing plasma levels, which was also verified in male to female and female to male transsexuals. On the other hand, sex differences in endothelin receptor density and higher binding capacity in men were reported (283). Furthermore, an increased receptor mediated vasoconstrictor tone was recently found in middle aged males, which might be an additional contributor to lower cardiovascular risk in normoglycemic women (284). However, in diabetic cells endothelin-1 expression is increased (285). Endothelin-1-mediated vasoconstriction in mesenteric artery rings was higher in female diabetic mice, whereas no sex differences were seen in newly manifested animals (286). However, diabetes induced cardiac remodeling in mice was increased in females at an earlier stage than in males. This was measured by prohypertrophic and prooxidant gene expression as well as cardiomyocyte size (287).
C. Coagulation
Further aspects, which could partly explain higher cardiovascular risk for women with T2DM compared with diabetic men, were described in a cross-sectional study, which documented in vitro sex differences in fibrin structure function (288). It is worth noting that diabetic women had a higher prothrombotic fibrin profile, with denser fibrin clots and prolonged fibrinolysis, which was shown in increased maximum absorbance, clot formation, and lysis time. These results were not changed after adjusting for higher plasminogen activator inhibitor 1 and fibrinogen levels, which were found in women. A further aggravation was described with increasing BMI and WCR, as well as lower HDL-cholesterol levels in diabetic women only. In men only, worse glycemic control was related to an increased atherothrombotic risk. Of note, increased fibrinolysis was only found in men at higher age, which could possibly be explained by decreasing PAI-1 levels with increasing age. In both sexes renal impairment, low glomerular filtration rate, smoking, and peripheral arterial occlusive disease, measured by ankle brachial index, were associated with increased atherothrombotic risk in T2DM, whereas for ischemic heart disease, a significant relation was found in men, with a trend shown in women. Sex-specific findings implicate a higher atherothrombotic risk for women with T2DM, which potentially could have clinical consequences. An individualized therapy strategy might be needed with more aggressive antithrombotic therapy in diabetic women and other higher risk groups, but a more cautious approach in older men, to minimize bleeding risk due to increased fibrinolysis. However, longitudinal and in vitro studies need to be undertaken to confirm these findings.
Another study investigating arteriogenesis in patients with stenotic or occluded coronary vessels, recently found that female sex and T2DM were independent risk factors for poor collateral vessel development in chronic total occlusion, in a collective of patients with severe coronary artery stenosis (289). Estrogen decline after menopause might be an underlying cause for women having worse outcome in this study. This hypothesis is corroborated by animal studies showing that angiogenesis was negatively influenced by estrogen loss in oophorectomized animals (290), whereas estrogen therapy induced collateral and microvascular remodeling in a similar animal model (291).
D. Cardiac energy supply
Although little is known about the glucose metabolism in the human heart, the energy supply through glucose in the diabetic heart is disturbed (292). Sex seems to influence glucose utilization in obese and diabetic subjects substantially (293, 294). In general, male hearts use more glucose, whereas female hearts prefer lipids (295). A recent study reports sex differences in intramyocardial glucose metabolism, assessed by positron emission tomography scans, with reduced intramyocardial glucose kinetics (ie, fractional glucose uptake and metabolism) in diabetic women compared with men. However, the reduction of glycogen synthesis, glycolysis, and glucose oxidation was more pronounced within the group of men, with decreasing levels from normal-weight to obese and T2DM group (296). The authors highlight that these sex differences have to be considered before starting metabolically active drugs, because higher plasma glucose levels were also associated with increased glucose kinetics, in diabetic patients, and this might have clinical relevance especially during ischemia. They suppose that mildly elevated plasma glucose levels in T2DM patients may improve glucose handling by the human heart and thus increase myocardial glucose metabolism.
E. Mortality
Presence of MetS was associated with a 2-fold higher risk of CVD and 1.5-fold increase of mortality, with consistently higher risk for women than men, including all-cause mortality (297). Diabetes is associated with an almost 2-fold increased risk of death (298). The sex ratio of risk of fatal CHD or stroke showed a greater risk in women, which did not improve over time (273, 274). An Italian register study found that diabetes increased the risk of first ever ischemic stroke by more than 50% in both men and women (299). Interestingly, this risk decreased with advancing age in both sexes but at a faster rate among men. Therefore, postmenopausal women at the age of 55–74 years were at higher risk for ischemic stroke than men of comparable age. Furthermore, the recurrence of stroke within the next years was increased by T2DM in women independent of age, whereas in diabetic men such enhancement was only observed in those younger than 70 years.
VII. Cardiomyopathy
Diabetic females feature greater susceptibility to diabetic cardiopathology besides CHD. They show greater wall thickness and left ventricular (LV) mass in relation to glycemic control (300) and diastolic dysfunction. This more closely relates to IGT, which is more relevant in women. Moreover, in another study, preclinical diabetic cardiomyopathy was common in diabetic patients, with female sex being the only independent predictor of LV hypertrophy (301). Preclinical diabetic cardiomyopathy was associated with adverse cardiac outcomes and higher mortality at follow-up. Obesity, hypertension and diabetes are all important and independent risk factors for heart failure and may cause more adverse impairment of myocardial metabolism in women compared with men (302, 303). A recent prospective cohort study confirms a positive association between BMI and heart failure risk among men, but suggests a J-shaped association among women with T2DM (304). Males tend to suffer more often of heart failure at younger age due to CVD. They are also more likely to develop myocardial dilatation, whereas women tend to develop hypertrophic cardiomyopathy with diastolic heart failure and preserved ejection fraction more often (305). Diabetes independently relates to nonischemic diabetic cardiomyopathy (306). A large-scale metaanalysis on heart failure, using a huge individual patient dataset, found that diabetes was more frequent in women than men, including patients with both reduced and preserved ejection fraction (307). Although in general a survival benefit was observed in women especially with nonischemic etiology, concomitant diabetes attenuated the lower risk of mortality related to female sex and modified the association between sex and deaths irrespective of a preserved or reduced LV function (307). Therefore, among diabetic patients no sex differences, according to all causes of death, could be described. Thus, diabetes appears to attenuate the otherwise protective effect of female sex on progression of cardiomyopathy, which is similar to the conditions in CVD, although the exact underlying mechanisms are still unclear. Besides lipotoxicity (see section V.N) many other molecular mechanisms are involved, including mitochondrial dysfunction, oxidative stress, intramyocardial inflammation, involvement of the reninangiotensin system, altered insulin signaling or female-specific cardiac glycogen handling as a response to metabolic stress (308), and sex-hormone related myocardial calcium handling (309). All these mechanisms can interact and impair cardiac function and promote cardiomyocyte injury (225). Above all, sex differences were shown in adrenergic response to physical activity with higher effects in women causing differences in lipid metabolism and myocardial hypertrophic action (310). However, most studies used animal models, and there is still a knowledge gap regarding sex dimorphism in human diabetic cardiomyopathy (311).
VIII. Diabetic Foot Syndrome
Men develop diabetic foot syndrome at earlier age and more frequently undergo lower extremity amputations (312, 313). Furthermore, data from a population-based Canadian cohort revealed that also all gender-socio- economic status interactions were of greater impact in males compared with females (314). Greatest disparity was seen between men in the lowest and women in the highest SES category. Positive predictors for a higher risk of foot ulcerations were previous ulcerations, the male sex, negative results at the monofilament test, missing of at least 1 pedal pulse and a longer duration of T2DM (315). However, the higher risk of men was not observed when assessing the population without a previous history of ulceration or amputation. In a cross-sectional study, patients with T2DM featured sex-specific differences in risk factors for peripheral arterial disease (316). In men age, BMI, and systolic BP, whereas in women age, uric acid levels, and insulin therapy, were independent risk factors for disease progression. Male sex, peripheral arterial disease and renal insufficiency are predictors of death in the long term (317). Studies highlighting sex dimorphism and exploring pathophysiological mechanisms in animal models or humans are widely missing. More research is needed to understand reported sex-specific differences and point out if disease progression is based on a sex-specific background.
IX. Diabetic Nephropathy
Men show faster progression of diabetic nephropathy and more often undergo dialysis therapy (318). However, diabetic women have a higher mortality risk than diabetic men during chronic dialysis treatment (Table 3) (319, 320). A clear sex and diabetes interaction effect was found resulting in excess mortality in diabetic women. A recent observational study investigating sex differences in target organ damage, in insulin-resistant patients, demonstrated increased vascular and renal damage in women, who had increased intima-media thickness progression, higher numbers of vascular plaques, and reduced pulse wave velocity compared with men (321). This was especially pronounced in T2DM women. Data from Australia and New Zealand corroborate a higher mortality risk in women, over 60 years of age and suffering from T2DM after first renal replacement therapy (322). This difference was not observed in the younger population. Increased mortality in diabetic women with end-stage renal disease, during the first 4 years after dialysis, was confirmed in a French population (323). Again older women were affected to a higher extent. However, actual data from the Swedish National Diabetes Register showed that excess mortality was much higher in females, younger than 55 years with advanced renal disease, than in men (324). In this study, increased risk of death from several causes, including cardiovascular reasons were also described at an older age and for milder stages of renal disease in diabetic women that included a further deterioration due to worsening of glycemic control.
Higher inflammation and greater oxidative stress in diabetic women with end-stage renal disease, as well as modifiable gender differences in access to and modalities of treatment involved, were identified in some of these studies partly explaining excess mortality in diabetic women (319–322).
In nondiabetic animal models, male sex featured faster progression of renal impairment, which was also corroborated by human studies (325, 326). Additional confirmation was given by another animal study showing more negative effects of androgens on glycemic control, BP, and endothelial and vascular response to endothelin-1, thromboxane or NO (327). In this study, the authors examined the effects of sex hormones on systematic and renal hemodynamic parameters, mean arterial pressure, renal cortical flow and renal medullary blood flow in castrated male and spayed female diabetic rats, compared with sham-operated animals. Mechanisms behind the consequences of castration resulting in endogenous androgen withdrawal were explained by effects on NO production, which is higher if testosterone is absent, and the endothelin B receptor, which may be directly influenced by testosterone and causes vasoconstriction. Interestingly, androgen blockade might have potential renal-protective effects, which was already shown in hypertensive male and female rat models treated with antiandrogens (328, 329).
In contrast, epidemiological cross-sectional data point to a higher risk of proteinuria and renal disease in women than men, among T2DM subjects (330). Furthermore, sex-specific differences in gene polymorphism are suggested by one study showing that diabetic women carrying ACE D allele have a higher risk for development of diabetic nephropathy, which was not seen in diabetic men (Table 2) (331). Notably, another study could prove sex dimorphism in endothelial function in patients with T2DM. In this study, women featured increased NO availability and reduced renal oxidative stress than their male counterparts, which might have protective effects on progression of diabetic renal impairment (332).
Sex hormones may be a key to explain these differences in men and women, generally suggesting that women are protected by estrogens, hindering the progression of nondiabetic renal disease at least before menopause (333). However, in diabetic subjects, this protection is alleviated. In contrast, testosterone accelerates the development of nondiabetic chronic renal disease, and in streptozotocin-induced diabetic male rats, decreased testosterone levels and changes of sex hormone levels exacerbated the development of diabetic nephropathy, showing the importance of sex hormones in pathophysiologic mechanisms behind disease progression (334).
X. Other Frequent Comorbidities
A. Functional limitations
In most clinical studies, women with T2DM show a higher burden of risk factors and comorbidities as well as more cognitive and physical functional limitations than males do (335, 336). Quantification of diabetes comorbidity risk across life, using nation-wide big claim data, further revealed age-related sex differences (335). More comorbidities in males were observed up to the age of 60 years, whereas more comorbidities in females thereafter. Additionally, worse glycemic control, higher BP and BMI, in combination with lower exercise levels directly mediated the association between sex and functional limitations in a large community-based T2DM cohort (336). Higher rates of depression, lower perceived family support and self-efficacy in women served as indirect mediators in this gender-functional limitations link. Overall, impaired cognitive function appears to affect self-care abilities to a greater extent in women.
In another population-based sample of older people, T2DM also exerted greater impact on the risk of geriatric conditions in women than in men (337). A greater proportion of diabetic women had cognitive impairment, depression, and falls than did diabetic men. Diabetes doubled the risk of these geriatric conditions among women, whereas no associations were found in diabetic men.
B. Mental disorders
Anxiety and eating disorders as well as depression are more common in diabetic subjects, especially in women (Table 3) (338). In addition, mental disorders adversely affect glycemic control, adherence to therapy, and development of complications. Furthermore, presence of depression doubles mortality risk in diabetic subjects (339). However, compared with nondiabetic subjects, the increase of the risk for depression seems even more pronounced in diabetic men. Nevertheless, diabetic men seem to live more effectively with their disease, showing lower prevalence of depression and anxiety, more active problem-oriented, and solving approach strategies, a better health-related quality of life and positive wellbeing (340).
C. Sexual function and reproduction
Diabetic males and females are prone to suffer from sexual dysfunctions and reproductive problems, which appear to be underestimated in clinical practice. Prepregnancy care in diabetic women of child-bearing age is still unsatisfying, due to consistently increasing rates of serious perinatal complications, including excess malformation rates and higher mortality (Table 3) (341). More than half of the investigated sexually active obese diabetic women and men complained about sexual dysfunction, which is much higher than in healthy lean subjects (342, 343). Sexual dysfunctions were strongly related to psychosocial factors and depressed mood in women but more to physiological factors, like cardiorespiratory fitness, glycemic control, and MetS in males. These problems may be regarded as markers for cardiovascular risk (344). Without it being clinically relevant the presence of erectile dysfunction can indicate doubling of new onset CVD events during the next decade, in middle-aged diabetic men (345). Impaired penile microcirculation may serve as an early marker of endothelial dysfunction, indicating higher cardiovascular risk. Additionally, males with erectile dysfunction commonly suffer from lower quality of life and depression.
XI. Future Perspective
Increased awareness of health professionals regarding sex and gender in development and management of T2DM and its complications is worthwhile. At present, there is evidence of many interesting sex and gender differences derived from both basic research and clinical studies. However, there are also many controversial issues and missing causalities in association studies. In addition, randomized controlled trials proving sex-specific effects by adequately designed interventions are widely missing. Appropriate animal models and translational research to study sex differences are needed to get more insight into the pathophysiology and complex interplay of hormones, genes, lifestyle, and environment. Ensuring consideration of female cells and animals in science, as well as of an adequate proportion of women in clinical studies that promote sex-specific analysis, including sex differences among the a priori research questions, is important for future biomedical research and medicine and could contribute to a better reproducibility of research (346).
Another problem is the lack of a defined methodology for sex- or gender-specific analysis (347). Sex and gender analysis is frequently performed by only applying subgroup analysis instead of more rigorous statistical procedures. Therefore, in order to detect and study complex sex and gender differences more efficiently and accurately in the future, analysis should focus on modifying factors as well as using different statistical approaches, including thorough power analysis.
In any case, information of potential sex differences regarding efficacy and tolerability of drugs are mandatory. An appropriate inclusion of pre- and postmenopausal women in early phase trials but also pregnant diabetic women and both elderly men and women in randomized controlled trials are necessary to guarantee high-quality research and healthcare for both sexes at all ages. Future studies should further elucidate the causes of attenuation of female vascular protection in diabetic women and possibilities to counteract. Better knowledge on protective mechanisms of one sex, for cardiometabolic and renal complications and psychological disorders, could help to establish new therapeutic strategies for both sexes. Furthermore, sex dimorphism in central insulin action could have clinical relevance in the treatment of obesity-related T2DM, which needs further investigation. Enhanced sex-specific genetic and epigenetic research could enable primary and secondary prevention giving more attention to the early phase of life, fetal sex, and parental behavioral factors. To push personalized individual care sex-specific screening programs and interventions have to be initiated and evaluated for their efficacy. Future guidelines for the management of T2DM, as well as its complications should consider sex and gender differences.
XII. Conclusions
One's sex is a fundamental biological factor, which plays a key role in regulation of homeostasis in health and causes vulnerability to cardiometabolic risk factors, as well as manifestation, clinical picture, and management of T2DM. Severity of injury differs in a sex-specific way regarding various diabetes-related comorbidities, especially cardiovascular and renal disease. Psychosocial factors also impact development and progression of diabetes and coping in a gender-dimorphic way. Reproductive factors and sexual function have to be considered. The care of diabetic pregnancy demands special attention, because this vulnerable phase programs health of offspring even in a sex-specific way. Otherwise hyperglycemic parents beget diabetic offspring, further contributing to pandemic increase of T2DM. Biomedical basic and clinical research in endocrinology should benefit both women and men in a balanced manner. Modern personalized treatment has to consider differences in biological factors, like genetic predisposition, sex hormones, and neurohumoral pathways, as well as behavioral and environmental differences between men and women.
Acknowledgments
We thank Anita Thomas for her assistance in preparation of the manuscript and Radka Tuskova and Stefano Sbrignadello for their support in the data collection and in the preparation and editing of the figures.
Author contributions: A.K.-W. wrote the article; J.H. and G.P. provided substantial contribution to the content; and all authors researched the data for the article and reviewed and/or edited the manuscript before submission.
Disclosure Summary: The authors have nothing to disclose.
Footnotes
- BAT
- brown adipose tissue
- BMI
- body mass index
- BP
- blood pressure
- BPA
- bisphenol A
- GGT
- γ-glutamyl transferase
- CHD
- coronary heart disease
- CVD
- cardiovascular disease
- ER
- estrogen receptor
- FA
- fatty acid
- GDM
- gestational diabetes mellitus
- GLP-1
- glucagon-like peptide-1
- HFD
- high-fat diet
- HDL
- high-density lipoprotein
- HPA
- hypothalamus-pituitary-adrenal
- IFG
- impaired fasting glucose
- IGM
- impaired glucose metabolism
- IGT
- impaired glucose tolerance
- IMCL
- intramyocellular lipids
- LBW
- low birth weight
- LV
- left ventricular
- MetS
- metabolic syndrome
- MI
- myocardial infarction
- MYCL
- myocardial lipids
- NGT
- normal glucose tolerance
- NO
- nitric oxide
- NPY
- neuropeptide Y
- PCOS
- polycystic ovary syndrome
- POMC
- proopiomelanocortin
- PPAR
- peroxisome proliferator-activated receptor
- SAT
- subcutaneous fat
- SES
- socioeconomic status
- SHBG
- sex hormone-binding globulin
- SSB
- sugar-sweetened beverage
- T2DM
- type 2 diabetes mellitus
- VAT
- visceral fat
- WCR
- waist circumference.
References
- 1. Schiebinger L, Klinge I, Sánchez de Madariaga I, Paik H, Schraudner M, Stefanick M. Gendered innovations in science, health, medicine, engineering and environment. 2011–2015. Available at http://genderedinnovations.stanford.edu/ Accessed January 10, 2015.
- 2. Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. EUGenMed Cardiovascular Clinical Study Group, Regitz-Zagrosek V, Oertelt-Prigione S, et al. Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes. Eur Heart J. 2016;37:24–34. [DOI] [PubMed] [Google Scholar]
- 4. Annandale E, Riska E. New connections: towards a gender-inclusive approach to women's and men's health. Curr Sociol. 2009;57:123–133. [Google Scholar]
- 5. Geary N. Counterpoint: physiologists should not distinguish “sex” and “gender.” Am J Physiol Regul Integr Comp Physiol. 2010;298:R1702–R1704. [DOI] [PubMed] [Google Scholar]
- 6. Hammarström A, Annandale E. A conceptual muddle: an empirical analysis of the use of ‘sex’ and ‘gender’ in ‘gender-specific medicine’ journals. PLoS One. 2012;7:e34193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wells JC, Marphatia AA, Cole TJ, McCoy D. Associations of economic and gender inequality with global obesity prevalence: understanding the female excess. Soc Sci Med. 2012;75:482–490. [DOI] [PubMed] [Google Scholar]
- 8. Pickett KE, Kelly S, Brunner E, Lobstein T, Wilkinson RG. Wider income gaps, wider waistbands? An ecological study of obesity and income inequality. J Epidemiol Community Health. 2005;59:670–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Garawi F, Devries K, Thorogood N, Uauy R. Global differences between women and men in the prevalence of obesity: is there an association with gender inequality? Eur J Clin Nutr. 2014;68:1101–1106. [DOI] [PubMed] [Google Scholar]
- 10. Zhang Q, Wang Y. Socioeconomic inequality of obesity in the United States: do gender, age, and ethnicity matter? Soc Sci Med. 2004;58:1171–1180. [DOI] [PubMed] [Google Scholar]
- 11. International Diabetes Federation. IDF Diabetes Atlas. 6th ed Brussels, Belgium: International Diabetes Federation; 2013. [Google Scholar]
- 12. Tobias M. Global control of diabetes: information for action. Lancet. 2011;378:3–4. [DOI] [PubMed] [Google Scholar]
- 13. Logue J, Walker JJ, Colhoun HM, et al. Do men develop type 2 diabetes at lower body mass indices than women? Diabetologia. 2011;54:3003–3006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wändell PE, Carlsson AC. Gender differences and time trends in incidence and prevalence of type 2 diabetes in Sweden–a model explaining the diabetes epidemic worldwide today? Diabetes Res Clin Pract. 2014;106:e90–e92. [DOI] [PubMed] [Google Scholar]
- 15. Bray GA. Medical consequences of obesity. J Clin Endocrinol Metab. 2004;89:2583–2589. [DOI] [PubMed] [Google Scholar]
- 16. Power ML, Schulkin J. Sex differences in fat storage, fat metabolism, and the health risks from obesity: possible evolutionary origins. Br J Nutr. 2008;99:931–940. [DOI] [PubMed] [Google Scholar]
- 17. Nielsen S, Guo Z, Johnson CM, Hensrud DD, Jensen MD. Splanchnic lipolysis in human obesity. J Clin Invest. 2004;113:1582–1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Westerbacka J, Cornér A, Tiikkainen M, et al. Women and men have similar amounts of liver and intra-abdominal fat, despite more subcutaneous fat in women: implications for sex differences in markers of cardiovascular risk. Diabetologia. 2004;47:1360–1369. [DOI] [PubMed] [Google Scholar]
- 19. He H, Ni Y, Chen J, et al. Sex difference in cardiometabolic risk profile and adiponectin expression in subjects with visceral fat obesity. Transl Res. 2010;155:71–77. [DOI] [PubMed] [Google Scholar]
- 20. Williams CM. Lipid metabolism in women. Proc Nutr Soc. 2004;63:153–160. [DOI] [PubMed] [Google Scholar]
- 21. Goodpaster BH, Krishnaswami S, Harris TB, et al. Obesity, regional body fat distribution, and the metabolic syndrome in older men and women. Arch Intern Med. 2005;165:777–783. [DOI] [PubMed] [Google Scholar]
- 22. Hu G, Bouchard C, Bray GA, et al. Trunk versus extremity adiposity and cardiometabolic risk factors in white and African American adults. Diabetes Care. 2011;34:1415–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Carr MC, Brunzell JD. Abdominal obesity and dyslipidemia in the metabolic syndrome: importance of type 2 diabetes and familial combined hyperlipidemia in coronary artery disease risk. J Clin Endocrinol Metab. 2004;89:2601–2607. [DOI] [PubMed] [Google Scholar]
- 24. Kuk JL, Lee S, Heymsfield SB, Ross R. Waist circumference and abdominal adipose tissue distribution: influence of age and sex. Am J Clin Nutr. 2005;81:1330–1334. [DOI] [PubMed] [Google Scholar]
- 25. Wannamethee SG, Papacosta O, Whincup PH, et al. Assessing prediction of diabetes in older adults using different adiposity measures: a 7 year prospective study in 6,923 older men and women. Diabetologia. 2010;53:890–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Meisinger C, Döring A, Thorand B, Heier M, ***Löwel H. Body fat distribution and risk of type 2 diabetes in the general population: are there differences between men and women? The MONICA/KORA Augsburg cohort study. Am J Clin Nutr. 2006;84:483–489. [DOI] [PubMed] [Google Scholar]
- 27. Schulze MB, Heidemann C, Schienkiewitz A, Bergmann MM, Hoffmann K, Boeing H. Comparison of anthropometric characteristics in predicting the incidence of type 2 diabetes in the EPIC-Potsdam study. Diabetes Care. 2006;29:1921–1923. [DOI] [PubMed] [Google Scholar]
- 28. Hartwig S, Greiser KH, Medenwald D, et al. Association of change of anthropometric measurements with incident type 2 diabetes mellitus: a pooled analysis of the prospective population-based CARLA and SHIP cohort studies. Medicine (Baltimore). 2015;94:e1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wang Q, Zhang M, Xu M, et al. Brown adipose tissue activation is inversely related to central obesity and metabolic parameters in adult human. PLoS One. 2015;10:e0123795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Grefhorst A, van den Beukel JC, van Houten EL, Steenbergen J, Visser JA, Themmen AP. Estrogens increase expression of bone morphogenetic protein 8b in brown adipose tissue of mice. Biol Sex Differ. 2015;6:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Liu X, Wang S, You Y, et al. Brown adipose tissue transplantation reverses obesity in ob/ob mice. Endocrinology. 2015;156:2461–2469. [DOI] [PubMed] [Google Scholar]
- 32. Mozumdar A, Liguori G. Persistent increase of prevalence of metabolic syndrome among U.S. adults: NHANES III to NHANES 1999–2006. Diabetes Care. 2011;34:216–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wannamethee SG, Papacosta O, Lawlor DA, et al. Do women exhibit greater differences in established and novel risk factors between diabetes and non-diabetes than men? The British Regional Heart Study and British Women's Heart Health Study. Diabetologia. 2012;55:80–87. [DOI] [PubMed] [Google Scholar]
- 34. Xu S, Gao B, Xing Y, et al. Gender differences in the prevalence and development of metabolic syndrome in Chinese population with abdominal obesity. PLoS One. 2013;8:e78270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Relimpio F, Martinez-Brocca MA, Leal-Cerro A, et al. Variability in the presence of the metabolic syndrome in type 2 diabetic patients attending a diabetes clinic. Influences of age and gender. Diabetes Res Clin Pract. 2004;65:135–142. [DOI] [PubMed] [Google Scholar]
- 36. Kuk JL, Ardern CI. Age and sex differences in the clustering of metabolic syndrome factors: association with mortality risk. Diabetes Care. 2010;33:2457–2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sattar N. Gender aspects in type 2 diabetes mellitus and cardiometabolic risk. Best Pract Res Clin Endocrinol Metab. 2013;27:501–507. [DOI] [PubMed] [Google Scholar]
- 38. Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379:2279–2290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. van Vliet-Ostaptchouk JV, Nuotio ML, Slagter SN, et al. The prevalence of metabolic syndrome and metabolically healthy obesity in Europe: a collaborative analysis of ten large cohort studies. BMC Endocr Disord. 2014;14:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bell JA, Kivimaki M, Hamer M. Metabolically healthy obesity and risk of incident type 2 diabetes: a meta-analysis of prospective cohort studies. Obes Rev. 2014;15:504–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chen GC, Qin LQ, Ye JK. Leptin levels and risk of type 2 diabetes: gender-specific meta-analysis. Obes Rev. 2014;15:134–142. [DOI] [PubMed] [Google Scholar]
- 42. Laughlin GA, Barrett-Connor E, Cummins KM, Daniels LB, Wassel CL, Ix JH. Sex-specific association of fetuin-A with type 2 diabetes in older community-dwelling adults: the Rancho Bernardo Study. Diabetes Care. 2013;36:1994–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Amitani M, Asakawa A, Amitani H, Inui A. The role of leptin in the control of insulin-glucose axis. Front Neurosci. 2013;7:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kadowaki T, Yamauchi T. Adiponectin and adiponectin receptors. Endocr Rev. 2005;26:439–451. [DOI] [PubMed] [Google Scholar]
- 45. Li S, Shin HJ, Ding EL, van Dam RM. Adiponectin levels and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2009;302:179–188. [DOI] [PubMed] [Google Scholar]
- 46. Bonneau GA, Pedrozo WR, Berg G. Adiponectin and waist circumference as predictors of insulin-resistance in women. Diabetes Metab Syndr. 2014;8:3–7. [DOI] [PubMed] [Google Scholar]
- 47. Rasul S, Ilhan A, Reiter MH, Baumgartner-Parzer S, Kautzky-Willer A. Relations of adiponectin to levels of metabolic parameters and sexual hormones in elderly type 2 diabetic patients. Gend Med. 2011;8:93–102. [DOI] [PubMed] [Google Scholar]
- 48. Abbasi A, Corpeleijn E, Meijer E, et al. Sex differences in the association between plasma copeptin and incident type 2 diabetes: the Prevention of Renal and Vascular Endstage Disease (PREVEND) study. Diabetologia. 2012;55:1963–1970. [DOI] [PubMed] [Google Scholar]
- 49. Daniels LB, Maisel AS. Cardiovascular biomarkers and sex: the case for women. Nat Rev Cardiol. 2015;12:588–596. [DOI] [PubMed] [Google Scholar]
- 50. Melander O, Maisel AS, Almgren P, et al. Plasma proneurotensin and incidence of diabetes, cardiovascular disease, breast cancer, and mortality. JAMA. 2012;308:1469–1475. [DOI] [PubMed] [Google Scholar]
- 51. Stadlmayr A, Aigner E, Huber-Schönauer U, et al. Relations of vitamin D status, gender and type 2 diabetes in middle-aged Caucasians. Acta Diabetol. 2015;52:39–46. [DOI] [PubMed] [Google Scholar]
- 52. Song Y, Wang L, Pittas AG, et al. Blood 25-hydroxy vitamin D levels and incident type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2013;36:1422–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lee BK, Park S, Kim Y. Age- and gender-specific associations between low serum 25-hydroxyvitamin D level and type 2 diabetes in the Korean general population: analysis of 2008–2009 Korean National Health and Nutrition Examination Survey data. Asia Pac J Clin Nutr. 2012;21:536–546. [PubMed] [Google Scholar]
- 54. Maestro B, Campión J, Dávila N, Calle C. Stimulation by 1,25-dihydroxyvitamin D3 of insulin receptor expression and insulin responsiveness for glucose transport in U-937 human promonocytic cells. Endocr J. 2000;47:383–391. [DOI] [PubMed] [Google Scholar]
- 55. Schneider AL, Lazo M, Ndumele CE, et al. Liver enzymes, race, gender and diabetes risk: the Atherosclerosis Risk in Communities (ARIC) study. Diabet Med. 2013;30:926–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hocking S, Samocha-Bonet D, Milner KL, Greenfield JR, Chisholm DJ. Adiposity and insulin resistance in humans: the role of the different tissue and cellular lipid depots. Endocr Rev. 2013;34:463–500. [DOI] [PubMed] [Google Scholar]
- 57. Pan JJ, Fallon MB. Gender and racial differences in nonalcoholic fatty liver disease. World J Hepatol. 2014;6:274–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Cicero AF, D'Addato S, Reggi A, Marchesini G, Borghi C. Gender difference in hepatic steatosis index and lipid accumulation product ability to predict incident metabolic syndrome in the historical cohort of the Brisighella Heart study. Metab Syndr Relat Disord. 2013;11:412–416. [DOI] [PubMed] [Google Scholar]
- 59. Buday B, Pach PF, Literati-Nagy B, et al. Sex influenced association of directly measured insulin sensitivity and serum transaminase levels: why alanine aminotransferase only predicts cardiovascular risk in men? Cardiovasc Diabetol. 2015;14:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ding EL, Song Y, Manson JE, et al. Sex hormone-binding globulin and risk of type 2 diabetes in women and men. N Engl J Med. 2009;361:1152–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Peter A, Kantartzis K, Machann J, et al. Relationships of circulating sex hormone-binding globulin with metabolic traits in humans. Diabetes. 2010;59:3167–3173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Mather KJ, Kim C, Christophi CA, et al. Steroid sex hormones, sex hormone-binding globulin, and diabetes incidence in the diabetes prevention program. J Clin Endocrinol Metab. 2015;100:3778–3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Mauvais-Jarvis F. Letter to the editor: “steroid sex hormones, sex hormone-binding globulin, and diabetes incidence in the diabetes prevention program” by Mather KJ, et al. J Clin Endocrinol Metab. 2015;100:L126–L127. [DOI] [PubMed] [Google Scholar]
- 64. Fenske B, Kische H, Gross S, et al. Endogenous androgens and sex hormone-binding globulin in women and risk of metabolic syndrome and type 2 diabetes. J Clin Endocrinol Metab. 2015:100:4595–4603. [DOI] [PubMed] [Google Scholar]
- 65. Varlamov O, Bethea CL, Roberts CT., Jr Sex-specific differences in lipid and glucose metabolism. Front Endocrinol (Lausanne). 2014;5:241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Mauvais-Jarvis F. Sex differences in metabolic homeostasis, diabetes, and obesity. Biol Sex Differ. 2015;6:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Lovejoy JC, Sainsbury A. Sex differences in obesity and the regulation of energy homeostasis. Obes Rev. 2009;10:154–167. [DOI] [PubMed] [Google Scholar]
- 68. Mauvais-Jarvis F, Clegg DJ, Hevener AL. The role of estrogens in control of energy balance and glucose homeostasis. Endocr Rev. 2013;34:309–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Navarro G, Allard C, Xu W, Mauvais-Jarvis F. The role of androgens in metabolism, obesity, and diabetes in males and females. Obesity (Silver Spring). 2015;23:713–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Elbers JM, Asscheman H, Seidell JC, Megens JA, Gooren LJ. Long-term testosterone administration increases visceral fat in female to male transsexuals. J Clin Endocrinol Metab. 1997;82:2044–2047. [DOI] [PubMed] [Google Scholar]
- 71. Ding EL, Song Y, Malik VS, Liu S. Sex differences of endogenous sex hormones and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2006;295:1288–1299. [DOI] [PubMed] [Google Scholar]
- 72. Jayasena CN, Franks S. The management of patients with polycystic ovary syndrome. Nat Rev Endocrinol. 2014;10:624–636. [DOI] [PubMed] [Google Scholar]
- 73. Moran LJ, Misso ML, Wild RA, Norman RJ. Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2010;16:347–363. [DOI] [PubMed] [Google Scholar]
- 74. Coviello AD, Sam S, Legro RS, Dunaif A. High prevalence of metabolic syndrome in first-degree male relatives of women with polycystic ovary syndrome is related to high rates of obesity. J Clin Endocrinol Metab. 2009;94:4361–4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Kobaly K, Vellanki P, Sisk RK, et al. Parent-of-origin effects on glucose homeostasis in polycystic ovary syndrome. J Clin Endocrinol Metab. 2014;99:2961–2966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Rao PM, Kelly DM, Jones TH. Testosterone and insulin resistance in the metabolic syndrome and T2DM in men. Nat Rev Endocrinol. 2013;9:479–493. [DOI] [PubMed] [Google Scholar]
- 77. Braun M, Wassmer G, Klotz T, Reifenrath B, Mathers M, Engelmann U. Epidemiology of erectile dysfunction: results of the ‘Cologne Male Survey.’ Int J Impot Res. 2000;12:305–311. [DOI] [PubMed] [Google Scholar]
- 78. Zitzmann M. Testosterone deficiency, insulin resistance and the metabolic syndrome. Nat Rev Endocrinol. 2009;5:673–681. [DOI] [PubMed] [Google Scholar]
- 79. Grossmann M. Low testosterone in men with type 2 diabetes: significance and treatment. J Clin Endocrinol Metab. 2011;96:2341–2353. [DOI] [PubMed] [Google Scholar]
- 80. Grossmann M. Testosterone and glucose metabolism in men: current concepts and controversies. J Endocrinol. 2014;220:R37–R55. [DOI] [PubMed] [Google Scholar]
- 81. Jones TH, Arver S, Behre HM, et al. Testosterone replacement in hypogonadal men with type 2 diabetes and/or metabolic syndrome (the TIMES2 study). Diabetes Care. 2011;34:828–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Unwin N, Shaw J, Zimmet P, Alberti KG. Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention. Diabet Med. 2002;19:708–723. [DOI] [PubMed] [Google Scholar]
- 83. Qiao Q. Comparison of different definitions of the metabolic syndrome in relation to cardiovascular mortality in European men and women. Diabetologia. 2006;49:2837–2846. [DOI] [PubMed] [Google Scholar]
- 84. Huang Y, Cai X, Chen P, et al. Associations of prediabetes with all-cause and cardiovascular mortality: a meta-analysis. Ann Med. 2014;46:684–692. [DOI] [PubMed] [Google Scholar]
- 85. Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373:1773–1779. [DOI] [PubMed] [Google Scholar]
- 86. Ratner RE, Christophi CA, Metzger BE, et al. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab. 2008;93:4774–4779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Buchanan TA, Xiang AH, Page KA. Gestational diabetes mellitus: risks and management during and after pregnancy. Nat Rev Endocrinol. 2012;8:639–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Persson M, Fadl H. Perinatal outcome in relation to fetal sex in offspring to mothers with pre-gestational and gestational diabetes–a population-based study. Diabet Med. 2014;31:1047–1054. [DOI] [PubMed] [Google Scholar]
- 89. Retnakaran R, Kramer CK, Ye C, et al. Fetal sex and maternal risk of gestational diabetes mellitus: the impact of having a boy. Diabetes Care. 2015;38:844–851. [DOI] [PubMed] [Google Scholar]
- 90. Retnakaran R, Shah BR. Fetal sex and the natural history of maternal risk of diabetes during and after pregnancy. J Clin Endocrinol Metab. 2015;100:2574–2580. [DOI] [PubMed] [Google Scholar]
- 91. Retnakaran R, Shah BR. Sex of the baby and future maternal risk of type 2 diabetes in women who had gestational diabetes. [published ahead of print October 15, 2015]. Diabet Med. 2015. doi: 10.1111/dme.12989. [DOI] [PubMed] [Google Scholar]
- 92. Lee DS, Kim YJ, Han HR. Sex differences in the association between socio-economic status and type 2 diabetes: data from the 2005 Korean National Health and Nutritional Examination Survey (KNHANES). Public Health. 2013;127:554–560. [DOI] [PubMed] [Google Scholar]
- 93. Kautzky-Willer A, Dorner T, Jensby A, Rieder A. Women show a closer association between educational level and hypertension or diabetes mellitus than males: a secondary analysis from the Austrian HIS. BMC Public Health. 2012;12:392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Tang M, Chen Y, Krewski D. Gender-related differences in the association between socioeconomic status and self-reported diabetes. Int J Epidemiol. 2003;32:381–385. [DOI] [PubMed] [Google Scholar]
- 95. Rathmann W, Haastert B, Icks A, et al. Sex differences in the associations of socioeconomic status with undiagnosed diabetes mellitus and impaired glucose tolerance in the elderly population: the KORA Survey 2000. Eur J Public Health. 2005;15:627–633. [DOI] [PubMed] [Google Scholar]
- 96. Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40:804–818. [DOI] [PubMed] [Google Scholar]
- 97. Rivera LA, Lebenbaum M, Rosella LC. The influence of socioeconomic status on future risk for developing type 2 diabetes in the Canadian population between 2011 and 2022: differential associations by sex. Int J Equity Health. 2015;14:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Maty SC, Lynch JW, Raghunathan TE, Kaplan GA. Childhood socioeconomic position, gender, adult body mass index, and incidence of type 2 diabetes mellitus over 34 years in the Alameda County Study. Am J Public Health. 2008;98:1486–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Krajnak KM. Potential contribution of work-related psychosocial stress to the development of cardiovascular disease and type II diabetes: a brief review. Environ Health Insights. 2014;8:41–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Eriksson AK, van den Donk M, Hilding A, Östenson CG. Work stress, sense of coherence, and risk of type 2 diabetes in a prospective study of middle-aged Swedish men and women. Diabetes Care. 2013;36:2683–2689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Norberg M, Stenlund H, Lindahl B, Andersson C, Eriksson JW, Weinehall L. Work stress and low emotional support is associated with increased risk of future type 2 diabetes in women. Diabetes Res Clin Pract. 2007;76:368–377. [DOI] [PubMed] [Google Scholar]
- 102. Heraclides AM, Chandola T, Witte DR, Brunner EJ. Work stress, obesity and the risk of type 2 diabetes: gender-specific bidirectional effect in the Whitehall II study. Obesity (Silver Spring). 2012;20:428–433. [DOI] [PubMed] [Google Scholar]
- 103. Pan A, Schernhammer ES, Sun Q, Hu FB. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med. 2011;8:e1001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Vetter C, Devore EE, Ramin CA, Speizer FE, Willett WC, Schernhammer ES. Mismatch of sleep and work timing and risk of type 2 diabetes. Diabetes Care. 2015;38:1707–1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Silva-Costa A, Rotenberg L, Nobre AA, Schmidt MI, Chor D, Griep RH. Gender-specific association between night-work exposure and type-2 diabetes: results from longitudinal study of adult health, ELSA-Brasil. Scand J Work Environ Health. 2015;41:568–578. [DOI] [PubMed] [Google Scholar]
- 106. Spaeth AM, Dinges DF, Goel N. Sex and race differences in caloric intake during sleep restriction in healthy adults. Am J Clin Nutr. 2014;100:559–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Gan Y, Yang C, Tong X, et al. Shift work and diabetes mellitus: a meta-analysis of observational studies. Occup Environ Med. 2015;72:72–78. [DOI] [PubMed] [Google Scholar]
- 108. Yu JH, Yun CH, Ahn JH, et al. Evening chronotype is associated with metabolic disorders and body composition in middle-aged adults. J Clin Endocrinol Metab. 2015;100:1494–1502. [DOI] [PubMed] [Google Scholar]
- 109. Lundberg U. Stress hormones in health and illness: the roles of work and gender. Psychoneuroendocrinology. 2005;30:1017–1021. [DOI] [PubMed] [Google Scholar]
- 110. Berntsson L, Lundberg U, Krantz G. Gender differences in work-home interplay and symptom perception among Swedish white-collar employees. J Epidemiol Community Health. 2006;60:1070–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. McEwen BS, Gray JD, Nasca C. 60 years of neuroendocrinology: redefining neuroendocrinology: stress, sex and cognitive and emotional regulation. J Endocrinol. 2015;226:T67–T83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Zhang B, Wing YK. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29:85–93. [DOI] [PubMed] [Google Scholar]
- 113. Schmid SM, Hallschmid M, Schultes B. The metabolic burden of sleep loss. Lancet Diabetes Endocrinol. 2015;3:52–62. [DOI] [PubMed] [Google Scholar]
- 114. Gangwisch JE, Feskanich D, Malaspina D, Shen S, Forman JP. Sleep duration and risk for hypertension in women: results from the nurses' health study. Am J Hypertens. 2013;26:903–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Cappuccio FP, Stranges S, Kandala NB, et al. Gender-specific associations of short sleep duration with prevalent and incident hypertension: the Whitehall II study. Hypertension. 2007;50:693–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33:414–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Huth C, Thorand B, Baumert J, et al. Job strain as a risk factor for the onset of type 2 diabetes mellitus: findings from the MONICA/KORA Augsburg cohort study. Psychosom Med. 2014;76:562–568. [DOI] [PubMed] [Google Scholar]
- 118. Leproult R, Holmbäck U, Van Cauter E. Circadian misalignment augments markers of insulin resistance and inflammation, independently of sleep loss. Diabetes. 2014;63:1860–1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Kriska AM, Edelstein SL, Hamman RF, et al. Physical activity in individuals at risk for diabetes: Diabetes Prevention Program. Med Sci Sports Exerc. 2006;38:826–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Nelson KM, Reiber G, Boyko EJ. Diet and exercise among adults with type 2 diabetes: findings from the third national health and nutrition examination survey (NHANES III). Diabetes Care. 2002;25:1722–1728. [DOI] [PubMed] [Google Scholar]
- 121. Meisinger C, Thorand B, Schneider A, Stieber J, Döring A, Löwel H. Sex differences in risk factors for incident type 2 diabetes mellitus: the MONICA Augsburg cohort study. Arch Intern Med. 2002;162:82–89. [DOI] [PubMed] [Google Scholar]
- 122. Ladabaum U, Mannalithara A, Myer PA, Singh G. Obesity, abdominal obesity, physical activity, and caloric intake in US adults: 1988 to 2010. Am J Med. 2014;127:717–727.e712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Hare-Bruun H, Flint A, Heitmann BL. Glycemic index and glycemic load in relation to changes in body weight, body fat distribution, and body composition in adult Danes. Am J Clin Nutr. 2006;84:871–879; quiz 952–873. [DOI] [PubMed] [Google Scholar]
- 124. Barclay AW, Petocz P, McMillan-Price J, et al. Glycemic index, glycemic load, and chronic disease risk–a meta-analysis of observational studies. Am J Clin Nutr. 2008;87:627–637. [DOI] [PubMed] [Google Scholar]
- 125. Pieroni L, Salmasi L. Fast-food consumption and body weight. Evidence from the UK. Food Policy. 2014;46:94–105. [Google Scholar]
- 126. Malik VS, Popkin BM, Bray GA, et al. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care. 2010;33:2477–2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Qi Q, Chu AY, Kang JH, et al. Sugar-sweetened beverages and genetic risk of obesity. N Engl J Med. 2012;367:1387–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Schulze MB, Manson JE, Ludwig DS, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA. 2004;292:927–934. [DOI] [PubMed] [Google Scholar]
- 129. Eshak ES, Iso H, Mizoue T, Inoue M, Noda M, Tsugane S. Soft drink, 100% fruit juice, and vegetable juice intakes and risk of diabetes mellitus. Clin Nutr. 2013;32:300–308. [DOI] [PubMed] [Google Scholar]
- 130. Singh GM, Micha R, Khatibzadeh S, Lim S, Ezzati M, Mozaffarian D. Estimated global, regional, and national disease burdens related to sugar-sweetened beverage consumption in 2010. Circulation. 2015;132:639–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Knott C, Bell S, Britton A. Alcohol consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of more than 1.9 million individuals from 38 observational studies. Diabetes Care. 2015;38:1804–1812. [DOI] [PubMed] [Google Scholar]
- 132. Schrieks IC, Heil AL, Hendriks HF, Mukamal KJ, Beulens JW. The effect of alcohol consumption on insulin sensitivity and glycemic status: a systematic review and meta-analysis of intervention studies. Diabetes Care. 2015;38:723–732. [DOI] [PubMed] [Google Scholar]
- 133. Rohwer RD, Liu S, You NC, Buring JE, Manson JE, Song Y. Interrelationship between alcohol intake and endogenous sex-steroid hormones on diabetes risk in postmenopausal women. J Am Coll Nutr. 2015;34:273–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2007;298:2654–2664. [DOI] [PubMed] [Google Scholar]
- 135. InterAct Consortium, Spijkerman AM, van der A DL, et al. Smoking and long-term risk of type 2 diabetes: the EPIC-InterAct study in European populations. Diabetes Care. 2014;37:3164–3171. [DOI] [PubMed] [Google Scholar]
- 136. Pan A, Wang Y, Talaei M, Hu FB, Wu T. Relation of active, passive, and quitting smoking with incident type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015;3:958–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Raho E, van Oostrom SH, Visser M, et al. Generation shifts in smoking over 20 years in two Dutch population-based cohorts aged 20–100 years. BMC Public Health. 2015;15:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet. 2011;378:1297–1305. [DOI] [PubMed] [Google Scholar]
- 139. Kaminsky Z, Wang SC, Petronis A. Complex disease, gender and epigenetics. Ann Med. 2006;38:530–544. [DOI] [PubMed] [Google Scholar]
- 140. Gluckman PD, Hanson MA, Cooper C, Thornburg KL. Effect of in utero and early-life conditions on adult health and disease. N Engl J Med. 2008;359:61–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Dunn GA, Morgan CP, Bale TL. Sex-specificity in transgenerational epigenetic programming. Horm Behav. 2011;59:290–295. [DOI] [PubMed] [Google Scholar]
- 142. Jimenez-Chillaron JC, Isganaitis E, Charalambous M, et al. Intergenerational transmission of glucose intolerance and obesity by in utero undernutrition in mice. Diabetes. 2009;58:460–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Ding GL, Wang FF, Shu J, et al. Transgenerational glucose intolerance with Igf2/H19 epigenetic alterations in mouse islet induced by intrauterine hyperglycemia. Diabetes. 2012;61:1133–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Jia Y, Cong R, Li R, et al. Maternal low-protein diet induces gender-dependent changes in epigenetic regulation of the glucose-6-phosphatase gene in newborn piglet liver. J Nutr. 2012;142:1659–1665. [DOI] [PubMed] [Google Scholar]
- 145. Yokomizo H, Inoguchi T, Sonoda N, et al. Maternal high-fat diet induces insulin resistance and deterioration of pancreatic β-cell function in adult offspring with sex differences in mice. Am J Physiol Endocrinol Metab. 2014;306:E1163–E1175. [DOI] [PubMed] [Google Scholar]
- 146. Samuelsson AM, Matthews PA, Argenton M, et al. Diet-induced obesity in female mice leads to offspring hyperphagia, adiposity, hypertension, and insulin resistance: a novel murine model of developmental programming. Hypertension. 2008;51:383–392. [DOI] [PubMed] [Google Scholar]
- 147. Huypens P, Sass S, Wu M, et al. Epigenetic germline inheritance of diet-induced obesity and insulin resistance. Nat Genet. 2016;48:497–499. [DOI] [PubMed] [Google Scholar]
- 148. Dearden L, Balthasar N. Sexual dimorphism in offspring glucose-sensitive hypothalamic gene expression and physiological responses to maternal high-fat diet feeding. Endocrinology. 2014;155:2144–2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Plagemann A. Perinatal Programming: The State of the Art. Berlin, Boston: De Gruyter; 2012. [Google Scholar]
- 150. Vogt MC, Paeger L, Hess S, et al. Neonatal insulin action impairs hypothalamic neurocircuit formation in response to maternal high-fat feeding. Cell. 2014;156:495–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Chong AC, Vogt MC, Hill AS, Brüning JC, Zeltser LM. Central insulin signaling modulates hypothalamus-pituitary-adrenal axis responsiveness. Mol Metab. 2015;4:83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Thurner S, Klimek P, Szell M, et al. Quantification of excess risk for diabetes for those born in times of hunger, in an entire population of a nation, across a century. Proc Natl Acad Sci USA. 2013;110:4703–4707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. de Rooij SR, Painter RC, Roseboom TJ, et al. Glucose tolerance at age 58 and the decline of glucose tolerance in comparison with age 50 in people prenatally exposed to the Dutch famine. Diabetologia. 2006;49:637–643. [DOI] [PubMed] [Google Scholar]
- 154. Ravelli AC, van der Meulen JH, Michels RP, et al. Glucose tolerance in adults after prenatal exposure to famine. Lancet. 1998;351:173–177. [DOI] [PubMed] [Google Scholar]
- 155. Tobi EW, Lumey LH, Talens RP, et al. DNA methylation differences after exposure to prenatal famine are common and timing- and sex-specific. Hum Mol Genet. 2009;18:4046–4053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Ravelli AC, van Der Meulen JH, Osmond C, Barker DJ, Bleker OP. Obesity at the age of 50 y in men and women exposed to famine prenatally. Am J Clin Nutr. 1999;70:811–816. [DOI] [PubMed] [Google Scholar]
- 157. Ericson U, Rukh G, Stojkovic I, et al. Sex-specific interactions between the IRS1 polymorphism and intakes of carbohydrates and fat on incident type 2 diabetes. Am J Clin Nutr. 2013;97:208–216. [DOI] [PubMed] [Google Scholar]
- 158. Aldhous MC, Reynolds RM, Campbell A, et al. Sex-differences in the metabolic health of offspring of parents with diabetes: a record-linkage study. PLoS One. 2015;10:e0134883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Wang C, Yatsuya H, Tamakoshi K, et al. Association between parental history of diabetes and the incidence of type 2 diabetes mellitus differs according to the sex of the parent and offspring's body weight: a finding from a Japanese worksite-based cohort study. Prev Med. 2015;81:49–53. [DOI] [PubMed] [Google Scholar]
- 160. Jaddoe VW, de Jonge LL, van Dam RM, et al. Fetal exposure to parental smoking and the risk of type 2 diabetes in adult women. Diabetes Care. 2014;37:2966–2973. [DOI] [PubMed] [Google Scholar]
- 161. Gabory A, Roseboom TJ, Moore T, Moore LG, Junien C. Placental contribution to the origins of sexual dimorphism in health and diseases: sex chromosomes and epigenetics. Biol Sex Differ. 2013;4:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Rosenfeld CS. Sex-specific placental responses in fetal development. Endocrinology. 2015;156:3422–3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Walsh JM, Segurado R, Mahony RM, Foley ME, McAuliffe FM. The effects of fetal gender on maternal and fetal insulin resistance. PLoS One. 2015;10:e0137215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Wilkin TJ, Murphy MJ. The gender insulin hypothesis: why girls are born lighter than boys, and the implications for insulin resistance. Int J Obes (Lond). 2006;30:1056–1061. [DOI] [PubMed] [Google Scholar]
- 165. Rodríguez G, Samper MP, Ventura P, Moreno LA, Olivares JL, Pérez-González JM. Gender differences in newborn subcutaneous fat distribution. Eur J Pediatr. 2004;163:457–461. [DOI] [PubMed] [Google Scholar]
- 166. Eder M, Csapo B, Wadsack C, et al. Sex differences in the association of cord blood insulin with subcutaneous adipose tissue in neonates. Int J Obes (Lond). 2016;40:538–542. [DOI] [PubMed] [Google Scholar]
- 167. Whincup PH, Kaye SJ, Owen CG, et al. Birth weight and risk of type 2 diabetes: a systematic review. JAMA. 2008;300:2886–2897. [DOI] [PubMed] [Google Scholar]
- 168. Johnsson IW, Haglund B, Ahlsson F, Gustafsson J. A high birth weight is associated with increased risk of type 2 diabetes and obesity. Pediatr Obes. 2015;10:77–83. [DOI] [PubMed] [Google Scholar]
- 169. Zimmermann E, Gamborg M, Sørensen TI, Baker JL. Sex differences in the association between birth weight and adult type 2 diabetes. Diabetes. 2015;64:4220–4225. [DOI] [PubMed] [Google Scholar]
- 170. Sato R, Watanabe H, Shirai K, et al. A cross-sectional study of glucose regulation in young adults with very low birth weight: impact of male gender on hyperglycaemia. BMJ Open. 2012;2:e000327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Richter VF, Briffa JF, Moritz KM, Wlodek ME, Hryciw DH. The role of maternal nutrition, metabolic function and the placenta in developmental programming of renal dysfunction. Clin Exp Pharmacol Physiol. 2016;43:135–141. [DOI] [PubMed] [Google Scholar]
- 172. Dalziel SR, Walker NK, Parag V, et al. Cardiovascular risk factors after antenatal exposure to betamethasone: 30-year follow-up of a randomised controlled trial. Lancet. 2005;365:1856–1862. [DOI] [PubMed] [Google Scholar]
- 173. Alexander N, Rosenlöcher F, Stalder T, et al. Impact of antenatal synthetic glucocorticoid exposure on endocrine stress reactivity in term-born children. J Clin Endocrinol Metab. 2012;97:3538–3544. [DOI] [PubMed] [Google Scholar]
- 174. Reynolds RM, Walker BR, Syddall HE, Andrew R, Wood PJ, Phillips DI. Is there a gender difference in the associations of birthweight and adult hypothalamic-pituitary-adrenal axis activity? Eur J Endocrinol. 2005;152:249–253. [DOI] [PubMed] [Google Scholar]
- 175. McCormick CM, Smythe JW, Sharma S, Meaney MJ. Sex-specific effects of prenatal stress on hypothalamic-pituitary-adrenal responses to stress and brain glucocorticoid receptor density in adult rats. Brain Res Dev Brain Res. 1995;84:55–61. [DOI] [PubMed] [Google Scholar]
- 176. Weinstock M, Matlina E, Maor GI, Rosen H, McEwen BS. Prenatal stress selectively alters the reactivity of the hypothalamic-pituitary adrenal system in the female rat. Brain Res. 1992;595:195–200. [DOI] [PubMed] [Google Scholar]
- 177. Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009;5:374–381. [DOI] [PubMed] [Google Scholar]
- 178. Doyle LW, Ford GW, Davis NM, Callanan C. Antenatal corticosteroid therapy and blood pressure at 14 years of age in preterm children. Clin Sci. 2000;98:137–142. [PubMed] [Google Scholar]
- 179. Lee DH, Porta M, Jacobs DR, Jr, Vandenberg LN. Chlorinated persistent organic pollutants, obesity, and type 2 diabetes. Endocr Rev. 2014;35:557–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Huang T, Saxena AR, Isganaitis E, James-Todd T. Gender and racial/ethnic differences in the associations of urinary phthalate metabolites with markers of diabetes risk: National Health and Nutrition Examination Survey 2001–2008. Environ Health. 2014;13:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Ashley-Martin J, Dodds L, Arbuckle TE, et al. A birth cohort study to investigate the association between prenatal phthalate and bisphenol A exposures and fetal markers of metabolic dysfunction. Environ Health. 2014;13:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Volberg V, Harley K, Calafat AM, et al. Maternal bisphenol a exposure during pregnancy and its association with adipokines in Mexican-American children. Environ Mol Mutagen. 2013;54:621–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Watkins DJ, Peterson KE, Ferguson KK, et al. Relating phthalate and BPA exposure to metabolism in peripubescence: the role of exposure timing, sex, and puberty. J Clin Endocrinol Metab. 2016:101:79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Jalouli M, Carlsson L, Améen C, et al. Sex difference in hepatic peroxisome proliferator-activated receptor α expression: influence of pituitary and gonadal hormones. Endocrinology. 2003;144:101–109. [DOI] [PubMed] [Google Scholar]
- 185. Yang X, Schadt EE, Wang S, et al. Tissue-specific expression and regulation of sexually dimorphic genes in mice. Genome Res. 2006;16:995–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Cvitic S, Longtine MS, Hackl H, et al. The human placental sexome differs between trophoblast epithelium and villous vessel endothelium. PLoS One. 2013;8:e79233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Shungin D, Winkler TW, Croteau-Chonka DC, et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature. 2015;518:187–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Babelova A, Burckhardt BC, Salinas-Riester G, Pommerenke C, Burckhardt G, Henjakovic M. Next generation sequencing of sex-specific genes in the livers of obese ZSF1 rats. Genomics. 2015;106:204–213. [DOI] [PubMed] [Google Scholar]
- 189. He T, Zhong PS, Cui Y. A set-based association test identifies sex-specific gene sets associated with type 2 diabetes. Front Genet. 2014;5:395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Chen X, McClusky R, Chen J, et al. The number of x chromosomes causes sex differences in adiposity in mice. PLoS Genet. 2012;8:e1002709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Bonthuis PJ, Rissman EF. Neural growth hormone implicated in body weight sex differences. Endocrinology. 2013;154:3826–3835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Voight BF, Scott LJ, Steinthorsdottir V, et al. Twelve type 2 diabetes susceptibility loci identified through large-scale association analysis. Nat Genet. 2010;42:579–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Guigas B, de Leeuw van Weenen JE, van Leeuwen N, et al. Sex-specific effects of naturally occurring variants in the dopamine receptor D2 locus on insulin secretion and type 2 diabetes susceptibility. Diabet Med. 2014;31:1001–1008. [DOI] [PubMed] [Google Scholar]
- 194. Ober C, Loisel DA, Gilad Y. Sex-specific genetic architecture of human disease. Nat Rev Genet. 2008;9:911–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Bonnefond A, Froguel P. Rare and common genetic events in type 2 diabetes: what should biologists know? Cell Metab. 2015;21:357–368. [DOI] [PubMed] [Google Scholar]
- 196. Walford GA, Porneala BC, Dauriz M, et al. Metabolite traits and genetic risk provide complementary information for the prediction of future type 2 diabetes. Diabetes Care. 2014;37:2508–2514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Ahrén B, Pacini G. Importance of quantifying insulin secretion in relation to insulin sensitivity to accurately assess β cell function in clinical studies. Eur J Endocrinol. 2004;150:97–104. [DOI] [PubMed] [Google Scholar]
- 198. Pacini G. The hyperbolic equilibrium between insulin sensitivity and secretion. Nutr Metab Cardiovasc Dis. 2006;16(suppl 1):S22–S27. [DOI] [PubMed] [Google Scholar]
- 199. Kautzky-Willer A, Brazzale AR, Tura A, et al. Gender effect on insulin sensitivity and secretion in different categories of glucose tolerance. Diabetologia. 2009;52:S210–S210. [Google Scholar]
- 200. Kautzky-Willer A, Brazzale AR, Moro E, et al. Influence of increasing BMI on insulin sensitivity and secretion in normotolerant men and women of a wide age span. Obesity (Silver Spring). 2012;20:1966–1973. [DOI] [PubMed] [Google Scholar]
- 201. Le May C, Chu K, Hu M, et al. Estrogens protect pancreatic β-cells from apoptosis and prevent insulin-deficient diabetes mellitus in mice. Proc Natl Acad Sci USA. 2006;103:9232–9237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Wong WP, Tiano JP, Liu S, et al. Extranuclear estrogen receptor-α stimulates NeuroD1 binding to the insulin promoter and favors insulin synthesis. Proc Natl Acad Sci USA. 2010;107:13057–13062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Ribas V, Nguyen MT, Henstridge DC, et al. Impaired oxidative metabolism and inflammation are associated with insulin resistance in ERα-deficient mice. Am J Physiol Endocrinol Metab. 2010;298:E304–E319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Alonso-Magdalena P, Ropero AB, Carrera MP, et al. Pancreatic insulin content regulation by the estrogen receptor ER α. PLoS One. 2008;3:e2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Pereira RI, Casey BA, Swibas TA, Erickson CB, Wolfe P, Van Pelt RE. Timing of estradiol treatment after menopause may determine benefit or harm to insulin action. J Clin Endocrinol Metab. 2015;100:4456–4462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Mascarenhas-Melo F, Marado D, Palavra F, et al. Diabetes abrogates sex differences and aggravates cardiometabolic risk in postmenopausal women. Cardiovasc Diabetol. 2013;12:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Steinberg HO, Paradisi G, Cronin J, et al. Type II diabetes abrogates sex differences in endothelial function in premenopausal women. Circulation. 2000;101:2040–2046. [DOI] [PubMed] [Google Scholar]
- 208. Peters SA, Huxley RR, Sattar N, Woodward M. Sex differences in the excess risk of cardiovascular diseases associated with type 2 diabetes: potential explanations and clinical implications. Curr Cardiovasc Risk Rep. 2015;9:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Harris MI, Flegal KM, Cowie CC, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. The Third National Health and Nutrition Examination Survey, 1988–1994. Diabetes Care. 1998;21:518–524. [DOI] [PubMed] [Google Scholar]
- 210. Pacini G, Mari A. Methods for clinical assessment of insulin sensitivity and β-cell function. Best Pract Res Clin Endocrinol Metab. 2003;17:305–322. [DOI] [PubMed] [Google Scholar]
- 211. Nauck MA. Glucagon-like peptide 1 (GLP-1) in the treatment of diabetes. Horm Metab Res. 2004;36:852–858. [DOI] [PubMed] [Google Scholar]
- 212. Færch K, Pacini G, Nolan JJ, Hansen T, Tura A, Vistisen D. Impact of glucose tolerance status, sex, and body size on glucose absorption patterns during OGTTs. Diabetes Care. 2013;36:3691–3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Phillips WT, Schwartz JG, McMahan CA. Rapid gastric emptying of an oral glucose solution in type 2 diabetic patients. J Nucl Med. 1992;33:1496–1500. [PubMed] [Google Scholar]
- 214. Jones KL, Russo A, Stevens JE, Wishart JM, Berry MK, Horowitz M. Predictors of delayed gastric emptying in diabetes. Diabetes Care. 2001;24:1264–1269. [DOI] [PubMed] [Google Scholar]
- 215. Basu R, Dalla Man C, Campioni M, et al. Effects of age and sex on postprandial glucose metabolism: differences in glucose turnover, insulin secretion, insulin action, and hepatic insulin extraction. Diabetes. 2006;55:2001–2014. [DOI] [PubMed] [Google Scholar]
- 216. Anderwald C, Gastaldelli A, Tura A, et al. Mechanism and effects of glucose absorption during an oral glucose tolerance test among females and males. J Clin Endocrinol Metab. 2011;96:515–524. [DOI] [PubMed] [Google Scholar]
- 217. Perseghin G, Scifo P, Pagliato E, et al. Gender factors affect fatty acids-induced insulin resistance in nonobese humans: effects of oral steroidal contraception. J Clin Endocrinol Metab. 2001;86:3188–3196. [DOI] [PubMed] [Google Scholar]
- 218. Moro C, Galgani JE, Luu L, et al. Influence of gender, obesity, and muscle lipase activity on intramyocellular lipids in sedentary individuals. J Clin Endocrinol Metab. 2009;94:3440–3447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Ortiz-Nieto F, Johansson L, Ahlström H, Weis J. Quantification of lipids in human lower limbs using yellow bone marrow as the internal reference: gender-related effects. Magn Reson Imaging. 2010;28:676–682. [DOI] [PubMed] [Google Scholar]
- 220. Tarnopolsky MA, Rennie CD, Robertshaw HA, Fedak-Tarnopolsky SN, Devries MC, Hamadeh MJ. Influence of endurance exercise training and sex on intramyocellular lipid and mitochondrial ultrastructure, substrate use, and mitochondrial enzyme activity. Am J Physiol Regul Integr Comp Physiol. 2007;292:R1271–R1278. [DOI] [PubMed] [Google Scholar]
- 221. Kautzky-Willer A, Krssak M, Winzer C, et al. Increased intramyocellular lipid concentration identifies impaired glucose metabolism in women with previous gestational diabetes. Diabetes. 2003;52:244–251. [DOI] [PubMed] [Google Scholar]
- 222. Prikoszovich T, Winzer C, Schmid AI, et al. Body and liver fat mass rather than muscle mitochondrial function determine glucose metabolism in women with a history of gestational diabetes mellitus. Diabetes Care. 2011;34:430–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223. Tian GX, Sun Y, Pang CJ, et al. Oestradiol is a protective factor for non-alcoholic fatty liver disease in healthy men. Obes Rev. 2012;13:381–387. [DOI] [PubMed] [Google Scholar]
- 224. Bozkurt L, Gobl CS, Tura A, et al. Fatty liver index predicts further metabolic deteriorations in women with previous gestational diabetes. PLoS One. 2012;7:e32710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. Bugger H, Abel ED. Molecular mechanisms of diabetic cardiomyopathy. Diabetologia. 2014;57:660–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Iozzo P, Lautamaki R, Borra R, et al. Contribution of glucose tolerance and gender to cardiac adiposity. J Clin Endocrinol Metab. 2009;94:4472–4482. [DOI] [PubMed] [Google Scholar]
- 227. Krššák M, Winhofer Y, Göbl C, et al. Insulin resistance is not associated with myocardial steatosis in women. Diabetologia. 2011;54:1871–1878. [DOI] [PubMed] [Google Scholar]
- 228. Winhofer Y, Krssak M, Wolf P, et al. Hepatic rather than cardiac steatosis relates to glucose intolerance in women with prior gestational diabetes. PLoS One. 2014;9:e91607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229. Palmer BF, Clegg DJ. The sexual dimorphism of obesity. Mol Cell Endocrinol. 2015;402:113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230. Karastergiou K, Smith SR, Greenberg AS, Fried SK. Sex differences in human adipose tissues - the biology of pear shape. Biol Sex Differ. 2012;3:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231. Brown LM, Gent L, Davis K, Clegg DJ. Metabolic impact of sex hormones on obesity. Brain Res. 2010;1350:77–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232. Anderson LA, McTernan PG, Barnett AH, Kumar S. The effects of androgens and estrogens on preadipocyte proliferation in human adipose tissue: influence of gender and site. J Clin Endocrinol Metab. 2001;86:5045–5051. [DOI] [PubMed] [Google Scholar]
- 233. Pedersen SB, Kristensen K, Hermann PA, Katzenellenbogen JA, Richelsen B. Estrogen controls lipolysis by up-regulating α2A-adrenergic receptors directly in human adipose tissue through the estrogen receptor α. Implications for the female fat distribution. J Clin Endocrinol Metab. 2004;89:1869–1878. [DOI] [PubMed] [Google Scholar]
- 234. Okura T, Koda M, Ando F, Niino N, Ohta S, Shimokata H. Association of polymorphisms in the estrogen receptor α gene with body fat distribution. Int J Obes Relat Metab Disord. 2003;27:1020–1027. [DOI] [PubMed] [Google Scholar]
- 235. Heine PA, Taylor JA, Iwamoto GA, Lubahn DB, Cooke PS. Increased adipose tissue in male and female estrogen receptor-α knockout mice. Proc Natl Acad Sci USA. 2000;97:12729–12734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236. Siiteri PK. Adipose tissue as a source of hormones. Am J Clin Nutr. 1987;45:277–282. [DOI] [PubMed] [Google Scholar]
- 237. Medrikova D, Jilkova ZM, Bardova K, Janovska P, Rossmeisl M, Kopecky J. Sex differences during the course of diet-induced obesity in mice: adipose tissue expandability and glycemic control. Int J Obes (Lond). 2012;36:262–272. [DOI] [PubMed] [Google Scholar]
- 238. Mårin P, Odén B, Björntorp P. Assimilation and mobilization of triglycerides in subcutaneous abdominal and femoral adipose tissue in vivo in men: effects of androgens. J Clin Endocrinol Metab. 1995;80:239–243. [DOI] [PubMed] [Google Scholar]
- 239. Finkelstein JS, Lee H, Burnett-Bowie SA, et al. Gonadal steroids and body composition, strength, and sexual function in men. N Engl J Med. 2013;369:1011–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240. Tilg H, Moschen AR. Microbiota and diabetes: an evolving relationship. Gut. 2014;63:1513–1521. [DOI] [PubMed] [Google Scholar]
- 241. Flak MB, Neves JF, Blumberg RS. Immunology. Welcome to the microgenderome. Science. 2013;339:1044–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242. Law J, Bloor I, Budge H, Symonds ME. The influence of sex steroids on adipose tissue growth and function. Horm Mol Biol Clin Investig. 2014;19:13–24. [DOI] [PubMed] [Google Scholar]
- 243. Vicennati V, Ceroni L, Genghini S, Patton L, Pagotto U, Pasquali R. Sex difference in the relationship between the hypothalamic-pituitary-adrenal axis and sex hormones in obesity. Obesity (Silver Spring). 2006;14:235–243. [DOI] [PubMed] [Google Scholar]
- 244. Gathercole LL, Lavery GG, Morgan SA, et al. 11β-hydroxysteroid dehydrogenase 1: translational and therapeutic aspects. Endocr Rev. 2013;34:525–555. [DOI] [PubMed] [Google Scholar]
- 245. Bailey M, Silver R. Sex differences in circadian timing systems: implications for disease. Front Neuroendocrinol. 2014;35:111–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Arnetz L, Rajamand Ekberg N, Brismar K, Alvarsson M. Gender difference in adrenal sensitivity to ACTH is abolished in type 2 diabetes. Endocr Connect. 2015;4:92–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247. Pasquali R. The hypothalamic-pituitary-adrenal axis and sex hormones in chronic stress and obesity: pathophysiological and clinical aspects. Ann NY Acad Sci. 2012;1264:20–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10:434–445. [DOI] [PubMed] [Google Scholar]
- 249. Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91:449–458. [DOI] [PubMed] [Google Scholar]
- 250. Wang GJ, Volkow ND, Telang F, et al. Evidence of gender differences in the ability to inhibit brain activation elicited by food stimulation. Proc Natl Acad Sci USA. 2009;106:1249–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251. Gold PW. The organization of the stress system and its dysregulation in depressive illness. Mol Psychiatry. 2015;20:32–47. [DOI] [PubMed] [Google Scholar]
- 252. Gobinath AR, Mahmoud R, Galea LA. Influence of sex and stress exposure across the lifespan on endophenotypes of depression: focus on behavior, glucocorticoids, and hippocampus. Front Neurosci. 2014;8:420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253. Kivimaki M, Batty GD, Hublin C. Shift work as a risk factor for future type 2 diabetes: evidence, mechanisms, implications, and future research directions. PLoS Med. 2011;8:e1001138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Eckel-Mahan K, Sassone-Corsi P. Metabolism and the circadian clock converge. Physiol Rev. 2013;93:107–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255. Bouatia-Naji N, Bonnefond A, Cavalcanti-Proença C, et al. A variant near MTNR1B is associated with increased fasting plasma glucose levels and type 2 diabetes risk. Nat Genet. 2009;41:89–94. [DOI] [PubMed] [Google Scholar]
- 256. Cipolla-Neto J, Amaral FG, Afeche SC, Tan DX, Reiter RJ. Melatonin, energy metabolism, and obesity: a review. J Pineal Res. 2014;56:371–381. [DOI] [PubMed] [Google Scholar]
- 257. Obayashi K, Saeki K, Tone N, et al. Lower melatonin secretion in older females: gender differences independent of light exposure profiles. J Epidemiol. 2015;25:38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258. Scheer FA, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci USA. 2009;106:4453–4458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259. Morris CJ, Yang JN, Garcia JI, et al. Endogenous circadian system and circadian misalignment impact glucose tolerance via separate mechanisms in humans. Proc Natl Acad Sci USA. 2015;112:E2225–E2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260. Nohara K, Zhang Y, Waraich RS, et al. Early-life exposure to testosterone programs the hypothalamic melanocortin system. Endocrinology. 2011;152:1661–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261. Shi H, Strader AD, Sorrell JE, Chambers JB, Woods SC, Seeley RJ. Sexually different actions of leptin in proopiomelanocortin neurons to regulate glucose homeostasis. Am J Physiol Endocrinol Metab. 2008;294:E630–E639. [DOI] [PubMed] [Google Scholar]
- 262. Clegg DJ, Brown LM, Woods SC, Benoit SC. Gonadal hormones determine sensitivity to central leptin and insulin. Diabetes. 2006;55:978–987. [DOI] [PubMed] [Google Scholar]
- 263. Clegg DJ, Riedy CA, Smith KA, Benoit SC, Woods SC. Differential sensitivity to central leptin and insulin in male and female rats. Diabetes. 2003;52:682–687. [DOI] [PubMed] [Google Scholar]
- 264. Keen-Rhinehart E, Desai M, Ross MG. Central insulin sensitivity in male and female juvenile rats. Horm Behav. 2009;56:275–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265. Lindtner C, Scherer T, Zielinski E, et al. Binge drinking induces whole-body insulin resistance by impairing hypothalamic insulin action. Sci Transl Med. 2013;5:170ra114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266. Brüning JC, Gautam D, Burks DJ, et al. Role of brain insulin receptor in control of body weight and reproduction. Science. 2000;289:2122–2125. [DOI] [PubMed] [Google Scholar]
- 267. Burke LK, Doslikova B, D'Agostino G, et al. Sex difference in physical activity, energy expenditure and obesity driven by a subpopulation of hypothalamic POMC neurons. Mol Metab. 2016;5:245–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268. Iwen KA, Scherer T, Heni M, et al. Intranasal insulin suppresses systemic but not subcutaneous lipolysis in healthy humans. J Clin Endocrinol Metab. 2014;99:E246–E251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269. Hallschmid M, Benedict C, Schultes B, Fehm HL, Born J, Kern W. Intranasal insulin reduces body fat in men but not in women. Diabetes. 2004;53:3024–3029. [DOI] [PubMed] [Google Scholar]
- 270. Anand SS, Islam S, Rosengren A, et al. Risk factors for myocardial infarction in women and men: insights from the INTERHEART study. Eur Heart J. 2008;29:932–940. [DOI] [PubMed] [Google Scholar]
- 271. Catalan M, Herreras Z, Pinyol M, et al. Prevalence by sex of preclinical carotid atherosclerosis in newly diagnosed type 2 diabetes. Nutr Metab Cardiovasc Dis. 2015;25:742–748. [DOI] [PubMed] [Google Scholar]
- 272. Onat A, Hergenç G, Keleş I, Doǧan Y, Türkmen S, Sansoy V. Sex difference in development of diabetes and cardiovascular disease on the way from obesity and metabolic syndrome. Metabolism. 2005;54:800–808. [DOI] [PubMed] [Google Scholar]
- 273. Peters SA, Huxley RR, Woodward M. Diabetes as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 64 cohorts, including 775,385 individuals and 12,539 strokes. Lancet. 2014;383:1973–1980. [DOI] [PubMed] [Google Scholar]
- 274. Peters SA, Huxley RR, Woodward M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia. 2014;57:1542–1551. [DOI] [PubMed] [Google Scholar]
- 275. Regitz-Zagrosek V. Therapeutic implications of the gender-specific aspects of cardiovascular disease. Nat Rev Drug Discov. 2006;5:425–438. [DOI] [PubMed] [Google Scholar]
- 276. Mendelsohn ME, Karas RH. Molecular and cellular basis of cardiovascular gender differences. Science. 2005;308:1583–1587. [DOI] [PubMed] [Google Scholar]
- 277. Dantas AP, Fortes ZB, de Carvalho MH. Vascular disease in diabetic women: why do they miss the female protection? Exp Diabetes Res. 2012;2012:570598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278. Cardillo C, Campia U, Bryant MB, Panza JA. Increased activity of endogenous endothelin in patients with type II diabetes mellitus. Circulation. 2002;106:1783–1787. [DOI] [PubMed] [Google Scholar]
- 279. Zhang R, Thor D, Han X, Anderson L, Rahimian R. Sex differences in mesenteric endothelial function of streptozotocin-induced diabetic rats: a shift in the relative importance of EDRFs. Am J Physiol Heart Circ Physiol. 2012;303:H1183–H1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280. Ortmann J, Veit M, Zingg S, et al. Estrogen receptor-α but not -β or GPER inhibits high glucose-induced human VSMC proliferation: potential role of ROS and ERK. J Clin Endocrinol Metab. 2011;96:220–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281. Smith EP, Boyd J, Frank GR, et al. Estrogen resistance caused by a mutation in the estrogen-receptor gene in a man. N Engl J Med. 1994;331:1056–1061. [DOI] [PubMed] [Google Scholar]
- 282. Sudhir K, Chou TM, Messina LM, et al. Endothelial dysfunction in a man with disruptive mutation in oestrogen-receptor gene. Lancet. 1997;349:1146–1147. [DOI] [PubMed] [Google Scholar]
- 283. Ergul A, Shoemaker K, Puett D, Tackett RL. Gender differences in the expression of endothelin receptors in human saphenous veins in vitro. J Pharmacol Exp Ther. 1998;285:511–517. [PubMed] [Google Scholar]
- 284. Stauffer BL, Westby CM, Greiner JJ, Van Guilder GP, Desouza CA. Sex differences in endothelin-1-mediated vasoconstrictor tone in middle-aged and older adults. Am J Physiol Regul Integr Comp Physiol. 2010;298:R261–R265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285. Gogg S, Smith U, Jansson PA. Increased MAPK activation and impaired insulin signaling in subcutaneous microvascular endothelial cells in type 2 diabetes: the role of endothelin-1. Diabetes. 2009;58:2238–2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286. Matsumoto T, Kakami M, Kobayashi T, Kamata K. Gender differences in vascular reactivity to endothelin-1 (1–31) in mesenteric arteries from diabetic mice. Peptides. 2008;29:1338–1346. [DOI] [PubMed] [Google Scholar]
- 287. Bowden MA, Tesch GH, Julius TL, Rosli S, Love JE, Ritchie RH. Earlier onset of diabesity-Induced adverse cardiac remodeling in female compared to male mice. Obesity (Silver Spring). 2015;23:1166–1177. [DOI] [PubMed] [Google Scholar]
- 288. Alzahrani SH, Hess K, Price JF, et al. Gender-specific alterations in fibrin structure function in type 2 diabetes: associations with cardiometabolic and vascular markers. J Clin Endocrinol Metab. 2012;97:E2282–E2287. [DOI] [PubMed] [Google Scholar]
- 289. Yetkin E, Topal E, Erguzel N, Senen K, Heper G, Waltenberger J. Diabetes mellitus and female gender are the strongest predictors of poor collateral vessel development in patients with severe coronary artery stenosis. Angiogenesis. 2015;18:201–207. [DOI] [PubMed] [Google Scholar]
- 290. Kyriakides ZS, Petinakis P, Kaklamanis L, et al. Gender does not influence angiogenesis and arteriogenesis in a rabbit model of chronic hind limb ischemia. Int J Cardiol. 2003;92:83–91. [DOI] [PubMed] [Google Scholar]
- 291. Lamping KG, Christensen LP, Tomanek RJ. Estrogen therapy induces collateral and microvascular remodeling. Am J Physiol Heart Circ Physiol. 2003;285:H2039–H2044. [DOI] [PubMed] [Google Scholar]
- 292. Peterson LR, Saeed IM, McGill JB, et al. Sex and type 2 diabetes: obesity-independent effects on left ventricular substrate metabolism and relaxation in humans. Obesity (Silver Spring). 2012;20:802–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293. Peterson LR, Soto PF, Herrero P, et al. Impact of gender on the myocardial metabolic response to obesity. JACC Cardiovasc Imaging. 2008;1:424–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294. Lyons MR, Peterson LR, McGill JB, et al. Impact of sex on the heart's metabolic and functional responses to diabetic therapies. Am J Physiol Heart Circ Physiol. 2013;305:H1584–H1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295. Peterson LR, Soto PF, Herrero P, Schechtman KB, Dence C, Gropler RJ. Sex differences in myocardial oxygen and glucose metabolism. J Nucl Cardiol. 2007;14:573–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296. Peterson LR, Herrero P, Coggan AR, et al. Type 2 diabetes, obesity, and sex difference affect the fate of glucose in the human heart. Am J Physiol Heart Circ Physiol. 2015;308:H1510–H1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297. Mottillo S, Filion KB, Genest J, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56:1113–1132. [DOI] [PubMed] [Google Scholar]
- 298. Emerging Risk Factors Collaboration, Seshasai SR, Kaptoge S, et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. 2011;364:829–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299. Policardo L, Seghieri G, Francesconi P, et al. Gender difference in diabetes-associated risk of first-ever and recurrent ischemic stroke. J Diabetes Complications. 2015;29:713–717. [DOI] [PubMed] [Google Scholar]
- 300. Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA. 1979;241:2035–2038. [DOI] [PubMed] [Google Scholar]
- 301. Kiencke S, Handschin R, von Dahlen R, et al. Pre-clinical diabetic cardiomyopathy: prevalence, screening, and outcome. Eur J Heart Fail. 2010;12:951–957. [DOI] [PubMed] [Google Scholar]
- 302. Kenchaiah S, Evans JC, Levy D, et al. Obesity and the risk of heart failure. N Engl J Med. 2002;347:305–313. [DOI] [PubMed] [Google Scholar]
- 303. Peterson LR, Herrero P, Schechtman KB, et al. Effect of obesity and insulin resistance on myocardial substrate metabolism and efficiency in young women. Circulation. 2004;109:2191–2196. [DOI] [PubMed] [Google Scholar]
- 304. Li W, Katzmarzyk PT, Horswell R, et al. Body mass index and heart failure among patients with type 2 diabetes. Circ Heart Fail. 2015;8:455–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305. Regitz-Zagrosek V, Brokat S, Tschope C. Role of gender in heart failure with normal left ventricular ejection fraction. Prog Cardiovasc Dis. 2007;49:241–251. [DOI] [PubMed] [Google Scholar]
- 306. Bertoni AG, Tsai A, Kasper EK, Brancati FL. Diabetes and idiopathic cardiomyopathy: a nationwide case-control study. Diabetes Care. 2003;26:2791–2795. [DOI] [PubMed] [Google Scholar]
- 307. Martínez-Sellés M, Doughty RN, Poppe K, et al. Gender and survival in patients with heart failure: interactions with diabetes and aetiology. Results from the MAGGIC individual patient meta-analysis. Eur J Heart Fail. 2012;14:473–479. [DOI] [PubMed] [Google Scholar]
- 308. Reichelt ME, Mellor KM, Curl CL, Stapleton D, Delbridge LM. Myocardial glycophagy - a specific glycogen handling response to metabolic stress is accentuated in the female heart. J Mol Cell Cardiol. 2013;65:67–75. [DOI] [PubMed] [Google Scholar]
- 309. Regitz-Zagrosek V, Oertelt-Prigione S, Seeland U, Hetzer R. Sex and gender differences in myocardial hypertrophy and heart failure. Circ J. 2010;74:1265–1273. [DOI] [PubMed] [Google Scholar]
- 310. Regitz-Zagrosek V, Dworatzek E, Kintscher U, Dragun D. Sex and sex hormone-dependent cardiovascular stress responses. Hypertension. 2013;61:270–277. [DOI] [PubMed] [Google Scholar]
- 311. Reichelt ME, Mellor KM, Bell JR, Chandramouli C, Headrick JP, Delbridge LM. Sex, sex steroids, and diabetic cardiomyopathy: making the case for experimental focus. Am J Physiol Heart Circ Physiol. 2013;305:H779–H792. [DOI] [PubMed] [Google Scholar]
- 312. Peek ME. Gender differences in diabetes-related lower extremity amputations. Clin Orthop Relat Res. 2011;469:1951–1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313. Bruun C, Siersma V, Guassora AD, Holstein P, de Fine Olivarius N. Amputations and foot ulcers in patients newly diagnosed with type 2 diabetes mellitus and observed for 19 years. The role of age, gender and co-morbidity. Diabet Med. 2013;30:964–972. [DOI] [PubMed] [Google Scholar]
- 314. Amin L, Shah BR, Bierman AS, et al. Gender differences in the impact of poverty on health: disparities in risk of diabetes-related amputation. Diabet Med. 2014;31:1410–1417. [DOI] [PubMed] [Google Scholar]
- 315. Crawford F, Cezard G, Chappell FM, et al. A systematic review and individual patient data meta-analysis of prognostic factors for foot ulceration in people with diabetes: the international research collaboration for the prediction of diabetic foot ulcerations (PODUS). Health Technol Assess. 2015;19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316. Tseng CH. Sex difference in the distribution of atherosclerotic risk factors and their association with peripheral arterial disease in Taiwanese type 2 diabetic patients. Circ J. 2007;71:1131–1136. [DOI] [PubMed] [Google Scholar]
- 317. Morbach S, Furchert H, Gröblinghoff U, et al. Long-term prognosis of diabetic foot patients and their limbs: amputation and death over the course of a decade. Diabetes Care. 2012;35:2021–2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318. de Hauteclocque A, Ragot S, Slaoui Y, et al. The influence of sex on renal function decline in people with Type 2 diabetes. Diabet Med. 2014;31:1121–1128. [DOI] [PubMed] [Google Scholar]
- 319. Carrero JJ, de Mutsert R, Axelsson J, et al. Sex differences in the impact of diabetes on mortality in chronic dialysis patients. Nephrol Dial Transplant. 2011;26:270–276. [DOI] [PubMed] [Google Scholar]
- 320. Hecking M, Bieber BA, Ethier J, et al. Sex-specific differences in hemodialysis prevalence and practices and the male-to-female mortality rate: the dialysis outcomes and practice patterns study (DOPPS). PLoS Med. 2014;11:e1001750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321. Gomez-Marcos MA, Recio-Rodriguez JI, Gomez-Sanchez L, et al. Gender differences in the progression of target organ damage in patients with increased insulin resistance: the LOD-DIABETES study. Cardiovasc Diabetol. 2015;14:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322. Villar E, Chang SH, McDonald SP. Incidences, treatments, outcomes, and sex effect on survival in patients with end-stage renal disease by diabetes status in Australia and New Zealand (1991 2005). Diabetes Care. 2007;30:3070–3076. [DOI] [PubMed] [Google Scholar]
- 323. Villar E, Remontet L, Labeeuw M, Ecochard R. Effect of age, gender, and diabetes on excess death in end-stage renal failure. J Am Soc Nephrol. 2007;18:2125–2134. [DOI] [PubMed] [Google Scholar]
- 324. Tancredi M, Rosengren A, Svensson AM, et al. Excess mortality among persons with type 2 diabetes. N Engl J Med. 2015;373:1720–1732. [DOI] [PubMed] [Google Scholar]
- 325. Remuzzi A, Puntorieri S, Mazzoleni A, Remuzzi G. Sex related differences in glomerular ultrafiltration and proteinuria in Munich-Wistar rats. Kidney Int. 1988;34:481–486. [DOI] [PubMed] [Google Scholar]
- 326. Silbiger SR, Neugarten J. The impact of gender on the progression of chronic renal disease. Am J Kidney Dis. 1995;25:515–533. [DOI] [PubMed] [Google Scholar]
- 327. Ajayi AA, Ogungbade GO, Okorodudu AO. Sex hormone regulation of systemic endothelial and renal microvascular reactivity in type-2 diabetes: studies in gonadectomized and sham-operated Zucker diabetic rats. Eur J Clin Invest. 2004;34:349–357. [DOI] [PubMed] [Google Scholar]
- 328. Baltatu O, Cayla C, Iliescu R, Andreev D, Bader M. Abolition of end-organ damage by antiandrogen treatment in female hypertensive transgenic rats. Hypertension. 2003;41:830–833. [DOI] [PubMed] [Google Scholar]
- 329. Baltatu O, Cayla C, Iliescu R, Andreev D, Jordan C, Bader M. Abolition of hypertension-induced end-organ damage by androgen receptor blockade in transgenic rats harboring the mouse ren-2 gene. J Am Soc Nephrol. 2002;13:2681–2687. [DOI] [PubMed] [Google Scholar]
- 330. Lin CH, Yang WC, Tsai ST, Tung TH, Chou P. A community-based study of chronic kidney disease among type 2 diabetics in Kinmen, Taiwan. Diabetes Res Clin Pract. 2007;75:306–312. [DOI] [PubMed] [Google Scholar]
- 331. Tien KJ, Hsiao JY, Hsu SC, et al. Gender-dependent effect of ACE I/D and AGT M235T polymorphisms on the progression of urinary albumin excretion in Taiwanese with type 2 diabetes. Am J Nephrol. 2009;29:299–308. [DOI] [PubMed] [Google Scholar]
- 332. Schneider MP, Ritt M, Raff U, Ott C, Schmieder RE. Gender is related to alterations of renal endothelial function in type 2 diabetes. Nephrol Dial Transplant. 2009;24:3354–3359. [DOI] [PubMed] [Google Scholar]
- 333. Maric C. Sex, diabetes and the kidney. Am J Physiol Renal Physiol. 2009;296:F680–F688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334. Xu Q, Wells CC, Garman JH, Asico L, Escano CS, Maric C. Imbalance in sex hormone levels exacerbates diabetic renal disease. Hypertension. 2008;51:1218–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335. McCollum M, Hansen LS, Lu L, Sullivan PW. Gender differences in diabetes mellitus and effects on self-care activity. Gend Med. 2005;2:246–254. [DOI] [PubMed] [Google Scholar]
- 336. Chiu CJ, Wray LA. Gender differences in functional limitations in adults living with type 2 diabetes: biobehavioral and psychosocial mediators. Ann Behav Med. 2011;41:71–82. [DOI] [PubMed] [Google Scholar]
- 337. Lu FP, Chang WC, Wu SC. Geriatric conditions, rather than multimorbidity, as predictors of disability and mortality among octogenarians: a population-based cohort study. Geriatr Gerontol Int. 2016;16:345–351. [DOI] [PubMed] [Google Scholar]
- 338. Young-Hyman DL, Davis CL. Disordered eating behavior in individuals with diabetes: importance of context, evaluation, and classification. Diabetes Care. 2010;33:683–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339. Sullivan MD, O'Connor P, Feeney P, et al. Depression predicts all-cause mortality: epidemiological evaluation from the ACCORD HRQL substudy. Diabetes Care. 2012;35:1708–1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340. Siddiqui MA, Khan MF, Carline TE. Gender differences in living with diabetes mellitus. Mater Sociomed. 2013;25:140–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341. Dabelea D, Mayer-Davis EJ, Lamichhane AP, et al. Association of intrauterine exposure to maternal diabetes and obesity with type 2 diabetes in youth: the SEARCH Case-Control study. Diabetes Care. 2008;31:1422–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342. Wing RR, Bond DS, Gendrano IN, 3rd, et al. Effect of intensive lifestyle intervention on sexual dysfunction in women with type 2 diabetes: results from an ancillary Look AHEAD study. Diabetes Care. 2013;36:2937–2944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343. Wing RR, Rosen RC, Fava JL, et al. Effects of weight loss intervention on erectile function in older men with type 2 diabetes in the Look AHEAD trial. J Sex Med. 2010;7:156–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344. Rosen RC, Wing RR, Schneider S, et al. Erectile dysfunction in type 2 diabetic men: relationship to exercise fitness and cardiovascular risk factors in the Look AHEAD trial. J Sex Med. 2009;6:1414–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345. Ma RC, So WY, Yang X, et al. Erectile dysfunction predicts coronary heart disease in type 2 diabetes. J Am Coll Cardiol. 2008;51:2045–2050. [DOI] [PubMed] [Google Scholar]
- 346. Collins FS, Tabak LA. Policy: NIH plans to enhance reproducibility. Nature. 2014;505:612–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347. Oertelt-Prigione S. Sex and gender in medical literature. In: Oertelt-Prigione S, Regitz-Zagrosek V, eds. Sex and Gender Aspects in Clinical Medicine. London, UK: Springer-Verlag; 2012:9–15. [Google Scholar]
- 348. World Health Organization. Raised fasting blood glucose (≥ 7.0 mmol/L or on medication). Data by country. Global Health Observatory Data Repository. 2015. Available at http://apps.who.int/gho/data/view.main.2469?lang=en Accessed November 18, 2015.
- 349. El Ati J, Traissac P, Delpeuch F, et al. Gender obesity inequities are huge but differ greatly according to environment and socio-economics in a North African setting: a national cross-sectional study in Tunisia. PLoS One. 2012;7:e48153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350. Coban N, Onat A, Yildirim O, Can G, Erginel-Unaltuna N. Oxidative stress-mediated (sex-specific) loss of protection against type-2 diabetes by macrophage migration inhibitory factor (MIF)-173G/C polymorphism. Clin Chim Acta. 2015;438:1–6. [DOI] [PubMed] [Google Scholar]
- 351. Fisher E, Li Y, Burwinkel B, et al. Preliminary evidence of FABP2 A54T polymorphism associated with reduced risk of type 2 diabetes and obesity in women from a German cohort. Horm Metab Res. 2006;38:341–345. [DOI] [PubMed] [Google Scholar]
- 352. Li Y, Fisher E, Klapper M, et al. Association between functional FABP2 promoter haplotype and type 2 diabetes. Horm Metab Res. 2006;38:300–307. [DOI] [PubMed] [Google Scholar]
- 353. Nordman S, Ding B, Ostenson CG, et al. Leu7Pro polymorphism in the neuropeptide Y (NPY) gene is associated with impaired glucose tolerance and type 2 diabetes in Swedish men. Exp Clin Endocrinol Diabetes. 2005;113:282–287. [DOI] [PubMed] [Google Scholar]
- 354. D'Adamo M, Perego L, Cardellini M, et al. The −866A/A genotype in the promoter of the human uncoupling protein 2 gene is associated with insulin resistance and increased risk of type 2 diabetes. Diabetes. 2004;53:1905–1910. [DOI] [PubMed] [Google Scholar]
- 355. Go MJ, Hwang JY, Park TJ, et al. Genome-wide association study identifies two novel Loci with sex-specific effects for type 2 diabetes mellitus and glycemic traits in a korean population. Diabetes Metab J. 2014;38:375–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356. McCarthy JJ, Somji A, Weiss LA, et al. Polymorphisms of the scavenger receptor class B member 1 are associated with insulin resistance with evidence of gene by sex interaction. J Clin Endocrinol Metab. 2009;94:1789–1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357. Simón I, Vendrell J, Gutiérrez C, et al. Pro12Ala substitution in the peroxisome proliferator-activated receptor-γ is associated with increased leptin levels in women with type-2 diabetes mellitus. Horm Res. 2002;58:143–149. [DOI] [PubMed] [Google Scholar]
- 358. Zietz B, Barth N, Spiegel D, Schmitz G, Schölmerich J, Schäffler A. Pro12Ala polymorphism in the peroxisome proliferator-activated receptor-γ2 (PPARγ2) is associated with higher levels of total cholesterol and LDL-cholesterol in male caucasian type 2 diabetes patients. Exp Clin Endocrinol Diabetes. 2002;110:60–66. [DOI] [PubMed] [Google Scholar]
- 359. Alkhalaf A, Landman GW, van Hateren KJ, et al. Sex specific association between carnosinase gene CNDP1 and cardiovascular mortality in patients with type 2 diabetes (ZODIAC-22). J Nephrol. 2015;28:201–207. [DOI] [PubMed] [Google Scholar]
- 360. Lee EY, Lee YH, Kim SH, et al. Association between heme oxygenase-1 promoter polymorphisms and the development of albuminuria in type 2 diabetes: a case-control study. Medicine (Baltimore). 2015;94:e1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361. Klimek P, Kautzky-Willer A, Chmiel A, Schiller-Frühwirth I, Thurner S. Quantification of diabetes comorbidity risks across life using nation-wide big claim data. PLoS Computer Biol. 2015;11:e1004125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362. Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with type 2 diabetes: a systematic review and meta-analysis. Diabet Med. 2006;23:1165–1173. [DOI] [PubMed] [Google Scholar]
- 363. Collins MM, Corcoran P, Perry IJ. Anxiety and depression symptoms in patients with diabetes. Diabet Med. 2009;26:153–161. [DOI] [PubMed] [Google Scholar]
- 364. Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. 2000;90:251–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365. Yang J, Cummings EA, O'connell C, Jangaard K. Fetal and neonatal outcomes of diabetic pregnancies. Obstet Gynecol. 2006;108:644–650. [DOI] [PubMed] [Google Scholar]
- 366. Kitahara CM, Flint AJ, Berrington de Gonzalez A, et al. Association between class III obesity (BMI of 40–59 kg/m2) and mortality: a pooled analysis of 20 prospective studies. PLoS Med. 2014;11:e1001673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367. Mari A, Pacini G, Murphy E, Ludvik B, Nolan JJ. A model-based method for assessing insulin sensitivity from the oral glucose tolerance test. Diabetes Care. 2001;24:539–548. [DOI] [PubMed] [Google Scholar]