Portal:Psychiatry/Selected article
Contents
Usage
- Add a new selected Article to the next available subpage.
- Update "max=" to new total for its {{Random portal component}} on the main page.
Selected Article
Major depressive disorder (MDD) (also known as clinical depression, major depression, unipolar depression, or unipolar disorder; or as recurrent depression in the case of repeated episodes) is a mental disorder characterized by a pervasive and persistent low mood that is accompanied by low self-esteem and by a loss of interest or pleasure in normally enjoyable activities. The term "depression" is used in a number of different ways. It is often used to mean this syndrome but may refer to other mood disorders or simple to a low mood. Major depressive disorder is a disabling condition that adversely affects a person's family, work or school life, sleeping and eating habits, and general health. In the United States, around 3.4% of people with major depression commit suicide, and up to 60% of people who commit suicide had depression or another mood disorder.
The diagnosis of major depressive disorder is based on the patient's self-reported experiences, behavior reported by relatives or friends, and a mental status examination. There is no laboratory test for major depression, although physicians generally request tests for physical conditions that may cause similar symptoms. The most common time of onset is between the ages of 20 and 30 years, with a later peak between 30 and 40 years. (Full article...)
Self-harm (SH) or deliberate self-harm (DSH) includes self-injury (SI) and self-poisoning and is defined as the intentional, direct injuring of body tissue most often done without suicidal intentions. These terms are used in the more recent literature in an attempt to reach a more neutral terminology. The older literature, especially that which predates the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR), almost exclusively refers to self-mutilation. The term self-harm is synonymous with the term self-injury.
The most common form of self-harm is skin-cutting but self-harm also covers a wide range of behaviors including, but not limited to, burning, scratching, banging or hitting body parts, interfering with wound healing (dermatillomania), hair-pulling (trichotillomania) and the ingestion of toxic substances or objects. Behaviours associated with substance abuse and eating disorders are usually not considered self-harm because the resulting tissue damage is ordinarily an unintentional side effect. However, the boundaries are not always clearly defined and in some cases behaviours that usually fall outside the boundaries of self-harm may indeed represent self-harm if performed with explicit intent to cause tissue damage. Although suicide is not the intention of self-harm, the relationship between self-harm and suicide is complex, as self-harming behaviour may be potentially life-threatening. There is also an increased risk of suicide in individuals who self-harm to the extent that self-harm is found in 40–60% of suicides. However, generalising self-harmers to be suicidal is, in the majority of cases, inaccurate. (Full article...)
Alzheimer's disease (AD), also known in medical literature as Alzheimer disease, is the most common form of dementia. There is no cure for the disease, which worsens as it progresses, and eventually leads to death. It was first described by German psychiatrist and neuropathologist Alois Alzheimer in 1906 and was named after him. Most often, AD is diagnosed in people over 65 years of age, although the less-prevalent early-onset Alzheimer's can occur much earlier. In 2006, there were 26.6 million people worldwide with AD. Alzheimer's is predicted to affect 1 in 85 people globally by 2050.
Although Alzheimer's disease develops differently for every individual, there are many common symptoms. Early symptoms are often mistakenly thought to be 'age-related' concerns, or manifestations of stress. In the early stages, the most common symptom is difficulty in remembering recent events, known as short term memory loss. When AD is suspected, the diagnosis is usually confirmed with tests that evaluate behaviour and thinking abilities, often followed by a brain scan if available, however, examination of brain tissue is required for a definitive diagnosis. As the disease advances, symptoms can include confusion, irritability, aggression, mood swings, trouble with language, and long-term memory loss. As the person's condition declines they often withdraw from family and society. Gradually, bodily functions are lost, ultimately leading to death. Since the disease is different for each individual, predicting how it will affect the person is difficult. AD develops for an unknown and variable amount of time before becoming fully apparent, and it can progress undiagnosed for years. On average, the life expectancy following diagnosis is approximately seven years. Fewer than 3% of individuals live more than 14 years after diagnosis. (Full article...)
Schizophrenia (/ˌskɪtsoʊˈfrɛniə/ or /ˌskɪtsoʊˈfriːniə/) is a mental disorder often characterized by abnormal social behavior and failure to recognize what is real. Common symptoms include false beliefs, unclear or confused thinking, auditory hallucinations, reduced social engagement and emotional expression, and inactivity. Diagnosis is based on observed behavior and the person's reported experiences.
Genetics and early environment, as well as psychological and social processes, appear to be important contributory factors. Some recreational and prescription drugs appear to cause or worsen symptoms. The many possible combinations of symptoms have triggered debate about whether the diagnosis represents a single disorder or a number of separate syndromes. Despite the origin of the term from the Greek roots skhizein ("to split") and phrēn ("mind"), schizophrenia does not imply a "split personality", or "multiple personality disorder"—a condition with which it is often confused in public perception. Rather, the term means a "splitting of mental functions", reflecting the presentation of the illness.
The mainstay of treatment is antipsychotic medication, which primarily suppresses dopamine receptor activity. Counseling, job training and social rehabilitation are also important in treatment. In more serious cases—where there is risk to self or others—involuntary hospitalization may be necessary, although hospital stays are now shorter and less frequent than they once were. (Full article...)
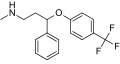
Sertraline (trade names Zoloft, Lustral) is an antidepressant of the selective serotonin reuptake inhibitor (SSRI) class. It was introduced to the market by Pfizer in 1991. Sertraline is primarily prescribed for major depressive disorder in adult outpatients as well as obsessive–compulsive, panic, and social anxiety disorders in both adults and children. In 2011, it was the second-most prescribed antidepressant on the U.S. retail market, with 37 million prescriptions.
Differences with other newer antidepressants are subtle and mostly confined to side effects. Evidence suggests that sertraline may work better than fluoxetine (Prozac) for some subtypes of depression. Treatment of panic disorder with sertraline results in a decrease of the number of panic attacks and an improved quality of life. For obsessive-compulsive disorder, sertraline is not as effective as cognitive behavioral therapy (CBT); the best results have been achieved by combining CBT with an SSRI. Sertraline is also effective for the treatment of social phobia and posttraumatic stress disorder. (Full article...)
Autism therapies attempt to lessen the deficits and abnormal behaviours associated with autism and other autism spectrum disorders (ASD), and to increase the quality of life and functional independence of autistic individuals, especially children. Treatment is typically catered to the child's needs. Treatments fall into two major categories: educational interventions and medical management. Training and support are also given to families of those with ASD.
Studies of interventions have methodological problems that prevent definitive conclusions about efficacy. Although many psychosocial interventions have some positive evidence, suggesting that some form of treatment is preferable to no treatment, the methodological quality of systematic reviews of these studies has generally been poor, their clinical results are mostly tentative, and there is little evidence for the relative effectiveness of treatment options. Intensive, sustained special education programs and behavior therapy early in life can help children with ASD acquire self-care, social, and job skills, and often can improve functioning, and decrease symptom severity and maladaptive behaviors; claims that intervention by around age three years is crucial are not substantiated. Available approaches include applied behavior analysis (ABA), developmental models, structured teaching, speech and language therapy, social skills therapy, and occupational therapy. Educational interventions have some effectiveness in children: intensive ABA treatment has demonstrated effectiveness in enhancing global functioning in preschool children, and is well established for improving intellectual performance of young children. Neuropsychological reports are often poorly communicated to educators, resulting in a gap between what a report recommends and what education is provided. The limited research on the effectiveness of adult residential programs shows mixed results. (Full article...)
Methylphenidate (trade names Concerta, Methylin, Ritalin, Equasym XL) is a substituted phenethylamine and psychostimulant drug used for the treatment of attention-deficit hyperactivity disorder (ADHD), postural orthostatic tachycardia syndrome and narcolepsy. Methylphenidate has been studied and researched for over 50 years and has a very good efficacy and safety record for the treatment of ADHD. The original patent was owned by CIBA, now Novartis Corporation. It was first licensed by the U.S. Food and Drug Administration (FDA) in 1955 for treating what was then known as hyperactivity. Prescribed to patients beginning in 1960, the drug became heavily prescribed in the 1990s, when the diagnosis of ADHD itself became more widely accepted.
ADHD and other similar conditions are believed to be linked to sub-performance of the dopamine and norepinephrine functions in the brain, primarily in the prefrontal cortex, responsible for self-regulatory function (e.g., inhibition, motivation, and memory) and executive function (e.g., reasoning, organizing, problem solving, and planning). Methylphenidate's mechanism of action involves the inhibition of catecholamine reuptake, primarily as a dopamine reuptake inhibitor. Methylphenidate acts by blocking the dopamine transporter and norepinephrine transporter, leading to increased concentrations of dopamine and norepinephrine within the synaptic cleft. This effect in turn leads to increased neurotransmission of dopamine and norepinephrine. (Full article...)
The Alaska Mental Health Enabling Act of 1956 (Public Law 84-830) was an Act of Congress passed to improve mental health care in the United States territory of Alaska. It became the focus of a major political controversy after opponents nicknamed it the "Siberia Bill" and denounced it as being part of a communist plot to hospitalize and brainwash Americans. Campaigners asserted that it was part of an international Jewish, Roman Catholic or psychiatric conspiracy intended to establish United Nations-run concentration camps in the United States.
The legislation in its original form was sponsored by the Democratic Party, but after it ran into opposition, it was rescued by the conservative Republican Senator Barry Goldwater. Under Goldwater's sponsorship, a version of the legislation without the commitment provisions that were the target of intense opposition from a variety of far-right, anti-Communist and fringe religious groups was passed by the United States Senate. The controversy still plays a prominent role in the Church of Scientology's account of its campaign against psychiatry. (Full article...)
In the Soviet Union, a systematic political abuse of psychiatry took place and was based on the interpretation of political dissent as a psychiatric problem. It was called "psychopathological mechanisms" of dissent.
During the leadership of General Secretary Leonid Brezhnev, psychiatry was used as a tool to eliminate political opponents ("dissidents") who openly expressed beliefs that contradicted official dogma. The term "philosophical intoxication" was widely used to diagnose mental disorders in cases where people disagreed with leaders and made them the target of criticism that used the writings by Karl Marx, Friedrich Engels, and Vladimir Lenin. Article 58-10 of the Stalin Criminal Code—which as Article 70 had been shifted into the RSFSR Criminal Code of 1962—and Article 190-1 of the RSFSR Criminal Code along with the system of diagnosing mental illness, developed by academician Andrei Snezhnevsky, created the very preconditions under which non-standard beliefs could easily be transformed into a criminal case, and it, in its turn, into a psychiatric diagnosis. Anti-Soviet political behavior, in particular, being outspoken in opposition to the authorities, demonstrating for reform, writing books were defined in some persons as being simultaneously a criminal act (e.g., violation of Articles 70 or 190-1), a symptom (e.g., "delusion of reformism"), and a diagnosis (e.g., "sluggish schizophrenia"). Within the boundaries of the diagnostic category, the symptoms of pessimism, poor social adaptation and conflict with authorities were themselves sufficient for a formal diagnosis of "sluggish schizophrenia." (Full article...)
Anti-psychiatry has been active for almost two centuries, and is the view that many psychiatric treatments are ultimately more damaging than helpful to patients. Psychiatry is seen by proponents of anti-psychiatry as a coercive instrument of oppression. According to anti-psychiatry, psychiatry involves an unequal power relationship between doctor and patient, and a highly subjective diagnostic process, leaving too much room for opinions and interpretations.
Anti-psychiatry originates in an objection to what some view as dangerous treatments. Examples include electroconvulsive therapy, insulin shock therapy, brain lobotomy, and the over-prescription of potentially dangerous pharmaceutical drugs. An immediate concern lies in the significant increase in prescribing psychiatric drugs for children. There were also concerns about mental health institutions. Every society, including liberal Western society, permits involuntary treatment or involuntary commitment of mental patients. (Full article...)
Amphetamine is a potent central nervous system (CNS) stimulant of the phenethylamine class that is used in the treatment of attention deficit hyperactivity disorder (ADHD) and narcolepsy. Amphetamine was discovered in 1887 and exists as two enantiomers: levoamphetamine and dextroamphetamine. Amphetamine properly refers to a specific chemical, the racemic free base, which is equal parts of the two enantiomers, levoamphetamine and dextroamphetamine, in their pure amine forms. However, the term is frequently used informally to refer to any combination of the enantiomers, or to either of them alone. Historically, it has been used to treat nasal congestion, depression, and obesity. Amphetamine is also used as a performance and cognitive enhancer, and recreationally as an aphrodisiac and euphoriant. It is a prescription medication in many countries, and unauthorized possession and distribution of amphetamine are often tightly controlled due to the significant health risks associated with uncontrolled or heavy use. (Full article...)
Bupropion (/bjuːˈproʊpi.ɒn/, bew-PROH-pee-on) is a drug primarily used as an antidepressant and smoking cessation aid. Marketed as Wellbutrin and Zyban among other trade names, it is one of the most frequently prescribed antidepressants in the United States, although in many English-speaking countries, including the United Kingdom, Australia and New Zealand, this is an off-label use. It is also widely used to aid people who are trying to quit smoking. It is taken in the form of tablets, and in the United States and most other countries it is available only with a prescription.
Clinically, bupropion serves as an atypical antidepressant fundamentally different from most commonly prescribed antidepressants such as selective serotonin reuptake inhibitors (SSRIs). It is an effective antidepressant on its own, but is also popular as an add-on medication in cases of incomplete response to first-line SSRI antidepressants. In contrast to many other antidepressants, it does not cause weight gain or sexual dysfunction. The most important side effect is an increase in risk for epileptic seizures, which caused the drug to be withdrawn from the market for some time and then caused the recommended dosage to be reduced. (Full article...)
Tourette syndrome (also called Tourette's syndrome, Tourette's disorder, Gilles de la Tourette syndrome, GTS or, more commonly, simply Tourette's or TS) is an inherited neuropsychiatric disorder with onset in childhood, characterized by multiple physical (motor) tics and at least one vocal (phonic) tic. These tics characteristically wax and wane, can be suppressed temporarily, and are preceded by a premonitory urge. Tourette's is defined as part of a spectrum of tic disorders, which includes provisional, transient and persistent (chronic) tics.
Tourette's was once considered a rare and bizarre syndrome, most often associated with the exclamation of obscene words or socially inappropriate and derogatory remarks (coprolalia), but this symptom is present in only a small minority of people with Tourette's. Tourette's is no longer considered a rare condition, but it is not always correctly identified because most cases are mild and the severity of tics decreases for most children as they pass through adolescence. Between 0.4% and 3.8% of children ages 5 to 18 may have Tourette's; the prevalence of other tic disorders in school-age children is higher, with the more common tics of eye blinking, coughing, throat clearing, sniffing, and facial movements. Extreme Tourette's in adulthood is a rarity, and Tourette's does not adversely affect intelligence or life expectancy. (Full article...)
Asperger syndrome (AS), also known as Asperger disorder (AD) or simply Asperger's, is an autism spectrum disorder (ASD) that is characterized by significant difficulties in social interaction and nonverbal communication, alongside restricted and repetitive patterns of behavior and interests. It differs from other autism spectrum disorders by its relative preservation of linguistic and cognitive development. Although not required for diagnosis, physical clumsiness and atypical (peculiar, odd) use of language are frequently reported. The diagnosis of Asperger's was eliminated in the 2013 fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and replaced by a diagnosis of autism spectrum disorder on a severity scale.
The syndrome is named after the Austrian pediatrician Hans Asperger who, in 1944, studied and described children in his practice who lacked nonverbal communication skills, demonstrated limited empathy with their peers, and were physically clumsy. The modern conception of Asperger syndrome came into existence in 1981 and went through a period of popularization, becoming standardized as a diagnosis in the early 1990s. Many questions and controversies remain about aspects of the disorder. There is doubt about whether it is distinct from high-functioning autism (HFA); partly because of this, its prevalence is not firmly established. (Full article...)
Autism is a disorder of neural development characterized by impaired social interaction, verbal and non-verbal communication, and by restricted and repetitive behavior. The diagnostic criteria require that symptoms become apparent before a child is three years old. Autism affects information processing in the brain by altering how nerve cells and their synapses connect and organize; how this occurs is not well understood. It is one of three recognized disorders in the autism spectrum (ASDs), the other two being Asperger syndrome, which lacks delays in cognitive development and language, and pervasive developmental disorder, not otherwise specified (commonly abbreviated as PDD-NOS), which is diagnosed when the full set of criteria for autism or Asperger syndrome are not met. (Full article...)
Suicide (Latin suicidium, from sui caedere, "to kill oneself") is the act of intentionally causing one's own death. Suicide is often carried out as a result of despair, the cause of which is frequently attributed to a mental disorder such as depression, bipolar disorder, schizophrenia, borderline personality disorder, alcoholism, or drug abuse. Stress factors such as financial difficulties or troubles with interpersonal relationships often play a role. Efforts to prevent suicide include limiting access to firearms, treating mental illness and drug misuse, and improving economic development. Although crisis hotlines are common, there is little evidence for their effectiveness. (Full article...)
Attention deficit hyperactivity disorder (ADHD, similar to hyperkinetic disorder in the ICD-10) is a psychiatric disorder in which there are significant problems of attention, hyperactivity, or acting impulsively that are not appropriate for a person's age. These symptoms must begin by age six to twelve and persist for more than six months for a diagnosis to be made. In school-aged individuals inattention symptoms often result in poor school performance.
Despite being the most commonly studied and diagnosed psychiatric disorder in children and adolescents, the cause in the majority of cases is unknown. It affects about 6–7% of children when diagnosed via the DSM-IV criteria and 1–2% when diagnosed via the ICD-10 criteria. Rates are similar between countries and depend mostly on how it is diagnosed. ADHD is diagnosed approximately three times more in boys than in girls. About 30–50% of people diagnosed in childhood continue to have symptoms into adulthood and between 2–5% of adults have the condition. The condition can be difficult to tell apart from other disorders as well as that of high normal activity. (Full article...)
A benzodiazepine /ˌbɛnzoʊdaɪˈæzᵻpiːn/ (sometimes colloquially "benzo"; often abbreviated "BZD") is a psychoactive drug whose core chemical structure is the fusion of a benzene ring and a diazepine ring. The first such drug, chlordiazepoxide (Librium), was discovered accidentally by Leo Sternbach in 1955, and made available in 1960 by Hoffmann–La Roche, which has also marketed the benzodiazepine diazepam (Valium) since 1963.
Benzodiazepines enhance the effect of the neurotransmitter gamma-aminobutyric acid (GABA) at the GABAA receptor, resulting in sedative, hypnotic (sleep-inducing), anxiolytic (anti-anxiety), anticonvulsant, and muscle relaxant properties; also seen in the applied pharmacology of high doses of many shorter-acting benzodiazepines are amnesic-dissociative actions. These properties make benzodiazepines useful in treating anxiety, insomnia, agitation, seizures, muscle spasms, alcohol withdrawal and as a premedication for medical or dental procedures. Benzodiazepines are categorized as either short-, intermediate-, or long-acting. Short- and intermediate-acting benzodiazepines are preferred for the treatment of insomnia; longer-acting benzodiazepines are recommended for the treatment of anxiety. (Full article...)
The mental status examination or mental state examination, abbreviated MSE, is an important part of the clinical assessment process in psychiatric practice. It is a structured way of observing and describing a patient's current state of mind, under the domains of appearance, attitude, behavior, mood and affect, speech, thought process, thought content, perception, cognition, insight and judgment. There are some minor variations in the subdivision of the MSE and the sequence and names of MSE domains.
The purpose of the MSE is to obtain a comprehensive cross-sectional description of the patient's mental state, which, when combined with the biographical and historical information of the psychiatric history, allows the clinician to make an accurate diagnosis and formulation, which are required for coherent treatment planning. (Full article...)
Gender identity disorder (GID) or gender dysphoria is the formal diagnosis used by psychologists and physicians to describe people who experience significant dysphoria (discontent) with the sex they were assigned at birth and/or the gender roles associated with that sex. Evidence suggests that people who identify with a gender different from the one they were assigned at birth may do so not just due to psychological or behavioral causes, but also biological ones related to their genetics, the makeup of their brains, or prenatal exposure to hormones.
Estimates of the prevalence of gender identity disorder range from a lower bound of 1:2000 (or about 0.05%) in the Netherlands and Belgium to 1.2% in New Zealand. Research indicates people who transition in adulthood are up to three times more likely to be male assigned at birth, but that among people transitioning in childhood the sex ratio is close to 1:1.
Gender identity disorder is classified as a medical disorder by the ICD-10 CM and DSM-5 (called gender dysphoria). Many transgender people and researchers support declassification of GID because they say the diagnosis pathologizes gender variance, reinforces the binary model of gender, and can result in stigmatization of transgender individuals. The official classification of gender dysphoria as a disorder in the DSM-5 may help resolve some of these issues, because the term "gender dysphoria" applies only to the discontent experienced by some persons resulting from gender identity issues.
The current medical approach to treatment for persons diagnosed with gender identity disorder is to support the individual in physically modifying the body to better match the psychological gender identity. This approach is based on the concept that their experience is based in a medical problem correctable by various forms of medical intervention. (Full article...)
Psychopathy (/saɪˈkɒpəθi/) (or sociopathy /ˈsoʊsiəˌpæθi/) is traditionally defined as a personality disorder characterized by enduring antisocial behavior, diminished empathy and remorse, and disinhibited or bold behavior. It may also be defined as a continuous aspect of personality, representing scores on different personality dimensions found throughout the population in varying combinations. The definition of psychopathy has varied significantly throughout the history of the concept; different definitions continue to be used that are only partly overlapping and sometimes appear contradictory.
The initial diagnostic criteria for antisocial personality reaction/disturbance is in the Diagnostic and Statistical Manual of Mental Disorders (DSM). The DSM and International Classification of Diseases (ICD) subsequently introduced the diagnoses of antisocial personality disorder (ASPD) and dissocial personality disorder, stating that these have been referred to (or include what is referred to) as psychopathy or sociopathy. Canadian psychologist Robert D. Hare later repopularised the construct of psychopathy in criminology with his Psychopathy Checklist. (Full article...)
Fluoxetine (also known by the trade names Prozac, Sarafem, Ladose and Fontex, among others) is an antidepressant of the selective serotonin reuptake inhibitor (SSRI) class. Fluoxetine was first documented in 1974 by scientists from Eli Lilly and Company. It was approved by the U.S. Food and Drug Administration for the treatment of major depressive disorder in December 1987. The U.S. fluoxetine patent expired in August 2001 and hence generic formulations are now available in the U.S..
Fluoxetine is used for the treatment of major depressive disorder (including pediatric depression), obsessive-compulsive disorder (in both adults and children), bulimia nervosa, panic disorder and premenstrual dysphoric disorder. In addition, fluoxetine is used to treat trichotillomania if cognitive behaviour therapy has been unsuccessful. (Full article...)
Psychosis (from the Greek ψυχή psyche, "mind/soul", and -ωσις -osis, "abnormal condition or derangement") refers to an abnormal condition of the mind, and is a generic psychiatric term for a mental state often described as involving a "loss of contact with reality". People with psychosis are described as psychotic. People experiencing psychosis may exhibit some personality changes and thought disorder. Depending on its severity, this may be accompanied by unusual or bizarre behavior, as well as difficulty with social interaction and impairment in carrying out daily life activities.
Psychosis (as a sign of a psychiatric disorder) is a diagnosis of exclusion. That is, a new-onset episode of psychosis is not considered a symptom of a psychiatric disorder until other relevant and known causes of psychosis are properly excluded. Medical and biological laboratory tests should exclude central nervous system diseases and injuries, diseases and injuries of other organs, psychoactive substances, toxins, and prescribed medications as causes of symptoms of psychosis before any psychiatric illness can be diagnosed. (Full article...)
Electroconvulsive therapy (ECT), formerly known as electroshock therapy and often referred to as shock treatment, is a standard psychiatric treatment in which seizures are electrically induced in patients to provide relief from psychiatric illnesses. ECT is usually used as a last line of intervention for major depressive disorder, schizophrenia, mania and catatonia. A usual course of ECT involves multiple administrations, typically given two or three times per week until the patient is no longer suffering symptoms. It was first introduced in 1938 by Italian neuropsychiatrists Ugo Cerletti and Lucio Bini, and gained widespread popularity among psychiatrists as a form of treatment in the 1940s and 1950s. (Full article...)
Substance abuse, also known as drug abuse, is a patterned use of a substance (drug) in which the user consumes the substance in amounts or with methods which are harmful to themselves or others. The exact cause of substance abuse is impossible to know because there is not just one direct cause. However substance abuse and addiction is known to run in families. One theory suggests there is a genetic disposition which predisposes certain individuals toward substance abuse. Another suggests substance abuse is learned there for people subjected to substance abuse by those around them begin to copy the same behaviors. Substance abuse might start out as a bad habit but when and if addiction develops it manifests as a chronic debilitating disease. (Full article...)
Bipolar disorder, also known as bipolar affective disorder (and originally called manic-depressive illness), is a mental disorder characterized by periods of elevated mood and periods of depression. The elevated mood is significant and is known as mania or hypomania depending on the severity or whether there is psychosis. During mania an individual feels or acts abnormally happy, energetic, or irritable. They often make poorly thought out decisions with little regard to the consequences. The need for sleep is usually reduced. During periods of depression there may be crying, poor eye contact with others, and a negative outlook on life. The risk of suicide among those with the disorder is high at greater than 6% over 20 years, while self harm occurs in 30–40%. Other mental health issues such as anxiety disorder and drug misuse are commonly associated. (Full article...)
The Diagnostic and Statistical Manual of Mental Disorders (DSM), published by the American Psychiatric Association, offers a common language and standard criteria for the classification of mental disorders. It is used, or relied upon, by clinicians, researchers, psychiatric drug regulation agencies, health insurance companies, pharmaceutical companies, the legal system, and policy makers together with alternatives such as the International Statistical Classification of Diseases and Related Health Problems (ICD), produced by the World Health Organization (WHO). The DSM is now in its fifth edition, DSM-5, published on May 18, 2013.
The DSM evolved from systems for collecting census and psychiatric hospital statistics, and from a United States Army manual. Revisions since its first publication in 1952 have incrementally added to the total number of mental disorders, although also removing those no longer considered to be mental disorders. (Full article...)
Portal:Psychiatry/Selected article/28
Portal:Psychiatry/Selected article/29