Rhabdomyosarcoma
| Rhabdomyosarcoma | |
|---|---|
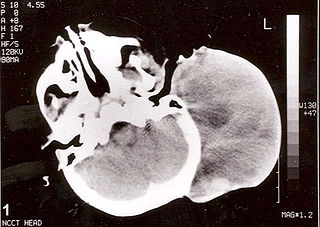
Non-contrast computed tomography of head showing a large mass without any intracranial extension. The diagnosis was postauricular congenital alveolar rhabdomyosarcoma.
|
|
| Classification and external resources | |
| Specialty | Oncology |
| ICD-10 | C49.M50 |
| ICD-9-CM | 171.9 |
| ICD-O | M8900/3-M8920/3 |
| OMIM | 268210 |
| DiseasesDB | 11485 |
| MedlinePlus | 001429 |
| eMedicine | ent/641 ped/2005 |
| Patient UK | Rhabdomyosarcoma |
| MeSH | D012208 |
A rhabdomyosarcoma, commonly referred to as RMS, is a type of cancer, specifically a sarcoma (cancer of connective tissues), in which the cancer cells are thought to arise from skeletal muscle progenitors. It can also be found attached to muscle tissue, wrapped around intestines, or in any anatomic location. It mostly occurs in areas naturally lacking in skeletal muscle, such as the head, neck, and genitourinary tract.
Contents
Presentation
Its two most common forms are embryonal rhabdomyosarcoma and alveolar rhabdomyosarcoma. In the former, which is more common in younger children, the cancer cells resemble those of a typical 6-to-8-week embryo. In the latter, which is more common in older children and teenagers, they resemble those of a typical 10-to-12-week embryo.
Epidemiology
Rhabdomyosarcoma is a relatively rare form of cancer. When RMS does occur, it is most commonly seen in children aged one to five years old. Less commonly, it can also present in teens aged 15 to 19, and can even develop in adulthood, though this is even more rare.
St. Jude Children's Research Hospital reports that Childhood Rhabdomyosarcoma is the most common soft tissue sarcoma in children. Soft tissue sarcomas make up about 3% of childhood cancers.
Diagnosis
The diagnosis of rhabdomyosarcoma is made by a pathologist; he or she will examine a biopsy of the tumor under the microscope and arrive at the diagnosis of rhabdomyosarcoma based on the morphology (appearance) of the tumor cells and the results of immunohistochemical stains.
Diagnosis of rhabdomyosarcoma depends on recognition of differentiation toward skeletal muscle cells. The proteins myoD1 and myogenin are transcription factor proteins normally found in developing skeletal muscle cells which disappears after the muscle matures and becomes innervated by a nerve. Thus, myoD1 and myogenin are not usually found in normal skeletal muscle and serve as a useful immunohistochemical marker of rhabdomyosarcoma.
Early manifestation can be misdiagnosed as a pseudotumor that is non responsive to steroid treatment.
MRI is the imaging modality of choice for the assessment of the primary adult rhabdomyosarcoma involving most body regions with additional value of diffusion weighted imaging and whole body MRI for staging.[3]
Classification
Several different histological subtypes of rhabdomyosarcoma exist, each of which has different clinical and pathological characteristics. Prognosis and clinical behavior of the tumor is also partially dependent on histologic subtype. Multiple classification systems have been proposed for subclassifying these tumors. The most recent classification system, the "International Classification of Rhabdomyosarcoma", was created by the Intergroup Rhabdomyosarcoma Study.[1] This system attempts to combine elements of the previous systems and correlate these with prognosis based on tumor type.
International Classification of Rhabdomyosarcoma
| Histologic Subtype | Prognosis |
|---|---|
| Botryoid Rhabdomyosarcoma | Superior Prognosis |
| Spindle cell rhabdomyosarcoma | Superior Prognosis |
| Embryonal rhabdomyosarcoma | Intermediate Prognosis |
| Alveolar rhabdomyosarcoma | Poor Prognosis |
| Undifferentiated Sarcoma | Poor Prognosis |
Several additional subtypes of rhabdomyosarcoma exist that do not fit into the International Classification scheme. Pleomorphic rhabdomyosarcoma usually occurs in adults rather than children, and, thus, is not included in this system. Sclerosing rhabdomyosarcoma is a rare rhabdomyosarcoma subtype recently characterized by Folpe, et al.; it is not included in this system.
Although botryoid and spindle cell rhabdomyosarcoma are classically considered as subtypes of embryonal rhabdomyosarcoma, they have more favorable clinical behavior and prognosis than classic embryonal rhabdomyosarcoma.
Treatment
Treatment for rhabdomyosarcoma consists of chemotherapy, radiation therapy and sometimes surgery. Surgery to remove the tumor may be difficult or impossible depending on the location of the tumor.
If there is no evidence of metastasis, surgery combined with chemotherapy and radiation offers the best prognosis. Patients whose tumors have not metastasized usually have a good chance for long-term survival, depending on the subtype of the tumor.
Batson Children's Hospital reports that more than 70% of children diagnosed with localized rhabdomyosarcoma have long-term survival.
Tungsten Alloy and RMS
A study has shown a link between RMS and Tungsten alloy embedded in muscle (e.g. bullet or missile fragments). [2] However, the tungsten alloy contained 6% Nickel, which is a known carcinogen. A synergistic effect of alloying tungsten with Ni is suggested (i.e. increasing the toxicity relative to either of the pure metals).
Research
Cancer stem cells of rhabdomyosarcoma have been identified and fibroblast growth factor receptor 3 has been suggested as their marker. Preclinical animal studies that try to use conditionally replicating adenoviruses against such cells are in progress. [3]
See also
References
- Lua error in package.lua at line 80: module 'strict' not found.
External links
- [1] A booklet for parents telling them about Rhabdomyosarcoma and what to do if you have a child with this type of cancer
- HP:1956 Rhabdomyosarcomas at humpath.com (Digital slides)
- Rhabdomyosarcoma by Leonard Wexler, MD in the Sarcoma Learning Center
- Ped-Onc Resource Center
- Information about Rhabdomyosarcoma from St. Jude Children's Research Hospital
- Lua error in package.lua at line 80: module 'strict' not found.
- http://www.healthsystem.virginia.edu/uvahealth/peds_oncology/rhabdo.cfm
