Abstract
A robust literature has documented the negative health effects of being the target of weight bias. Weight bias internalization (WBI) occurs when individuals apply negative weight stereotypes to themselves and self-derogate because of their body weight. Compared to experiences of weight bias, less is known about the relationship between WBI and mental and physical health, although more literature on this topic has emerged in recent years. The current systematic review identified 74 studies assessing the relationship between WBI and health, and interventions designed to reduce WBI and improve health. Over half of identified studies were published from 2016–2017. Results showed strong, negative relationships between WBI and mental health outcomes. Fewer studies have examined the relationship between WBI and physical health, and results were less consistent. Key directions for future research are highlighted, including the need for prospective and experimental studies with greater sample diversity.
Keywords: Health, obesity, stigma, weight bias internalization
Introduction
Weight bias refers to negative attitudes directed toward individuals who are perceived to have excess body weight. These prejudicial attitudes are rooted in negative stereotypes, including views that people with obesity are lazy, incompetent, and lack willpower.1 Weight bias can lead to overt forms of unfair treatment (i.e., discrimination) in employment, education, and health care, as well as stigma in interpersonal relationships and the mass media.2 Thus, individuals with obesity are vulnerable to social stigma – or societal devaluation and derogation – due to their weight in an array of settings and from multiple sources. Several systematic reviews and meta-analyses have described the prevalence and negative health consequences of experiencing weight discrimination and stigma.3–6
The internalization of negative weight stereotypes and subsequent self-disparagement – known as weight bias internalization (WBI), or self-directed weight stigma7 – has received less empirical attention than weight bias and stigma as expressed and enacted by others.8 Internalized stigma is broadly defined as (1) awareness of negative stereotypes about one’s social identity; (2) agreement with these stereotypes; (3) application of these stereotypes to oneself; and (4) self-devaluation due to one’s social identity.9 Recent estimates suggest that 40% of US adults with overweight and obesity have internalized weight bias, and 20% show high levels of WBI.10 Considering that two-thirds of US adults11 and one-third of youth12 have overweight/obesity, the pervasiveness of WBI is striking.
Prior research on other stigmatized social identities (due to mental illness, sexual orientation, and race) suggests that internalized stigma is associated with negative mental and physical health outcomes.13–15 To date, no systematic review has been conducted to comprehensively synthesize and evaluate the evidence on WBI and health. To address this gap, we critically reviewed existing literature examining the relationship between WBI and mental and physical health, as well as interventions to reduce WBI and improve health. In addition, our review identifies limitations of prior research and highlights key research needs that can inform priorities for future studies.
Methods
Data collection and synthesis for this literature review were conducted in accordance with PRISMA guidelines for systematic reviews.16
Eligibility Criteria
Studies were required to include at least one measure of WBI and at least one measure of mental or physical health. Measures of WBI were required to adequately assess the construct as defined above; measures that only assessed one aspect of WBI (e.g., stereotype awareness or agreement) were excluded. Other inclusion criteria included: published in a peer-reviewed journal; written in English; and included quantitative analysis of the relationship between WBI and health. Review papers, conceptual and commentary pieces, and qualitative studies were excluded. Abstracts from conference proceedings, dissertations/theses, and chapters were also excluded from this review.
Search Strategy
Five electronic databases (PubMed, SCOPUS, ScienceDirect, EMBASE, and PsycInfo) were searched in November 2017. Searches were conducted to include articles with any of the following terms in the title, abstract, or keywords: weight bias internalization; weight bias internalisation; internalized weight bias; internalised weight bias; internalized weight stigma; internalised weight stigma; self-directed weight stigma; self-directed weight bias; weight self-stigma.
Study Selection
Duplicate studies were removed before screening titles and abstracts for exclusion/inclusion criteria. As depicted in Figure 1, initial screening eliminated review/conceptual/commentary papers, papers not published in English, papers that were not related to weight or weight bias, and publications that were not full-text articles (e.g., abstracts only). More thorough screening was used for the remaining articles to further exclude papers that did not include quantitative analyses of measures of WBI and health. Additional articles identified during the course of screening the selected studies were also included.
Figure 1.
Flow diagram for study selection
Data Abstraction and Synthesis
We extracted the following data across all studies: country of origin; sample size, type (e.g., community versus clinical), and demographic characteristics; study design; study measures; and main study outcomes. Studies were divided into four categories: 1) WBI and adult mental health outcomes; 2) WBI and adult physical health outcomes; 3) studies of WBI in youth; and 4) interventions to reduce WBI. Descriptive statistics were computed for the number of studies published per year, basic characteristics of the studies, measures included in the studies, and main findings regarding WBI and health. Effect sizes (e.g., r values from correlations) and other relevant statistical coefficients (e.g., p values) were abstracted for key findings.
Quality Assessment
Apriori sources of bias were identified based on criteria from established quality assessment checklists.17,18 However, due to the limited number of rigorous research designs (e.g., longitudinal or experimental) in the current literature, criteria were modified based on the authors’ prior knowledge of research on WBI. Quality assessment of studies included in this review addressed the following factors: sample diversity, with respect to race/ethnicity and gender; cross-sectional versus longitudinal study design; observational versus experimental design; self-report versus objective measurement; and validity of the WBI measure.
Results
Figure 1 presents the study selection flow. Across all five databases, 308 studies were identified. Four additional studies were identified during the process of screening the selected studies (e.g., identifying relevant studies in the listed references of articles). After duplicates were removed, 153 titles and abstracts were screened, after which 115 full texts were reviewed for final evaluation of inclusion/exclusion criteria. Forty-one of these studies were excluded for lack of measures assessing WBI and/or health (n=36), or for being strictly qualitative (n=5), resulting in 74 studies that comprised the total sample for final analyses.
Characteristics and Quality of Studies
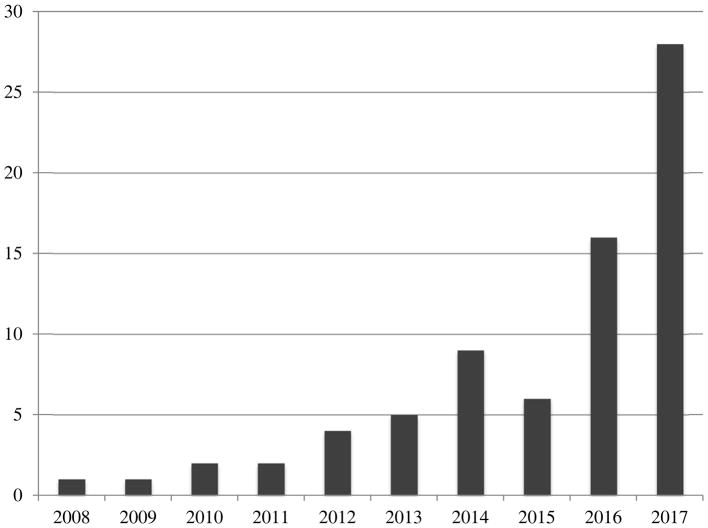
Figure 2 displays the number of studies published per year. The first study was published in 2008 and the majority of studies (59.5%) were published between 2016 and 2017. Over half (52.7%) of study samples consisted of ≥75% women, and 22.2% did not include men at all. More than one-third of samples (37.5%) consisted of ≥75% white participants, and an additional 23.0% of studies did not report race but were conducted in predominantly white countries (e.g., sample comprised 100% German nationality). Thus, over 60% of the study samples were limited in racial and ethnic diversity.
Figure 2.
Number of published studies on weight bias internalization and health per year
Three-quarters (75.7%) of studies were cross-sectional. Most longitudinal or experimental studies reported baseline associations between WBI and health outcomes as well. Therefore, the vast majority of published evidence relies heavily on cross-sectional data. Five studies presented data from behavioral weight loss or healthy eating trials,19–23 and seven tested interventions targeting WBI with up to 3 month follow-up.24–30 Aside from these intervention trials, only two experimental studies tested the causes and consequences of WBI.31,32 Three additional studies were observational, longitudinal studies,33–35 and one study used ecological momentary assessment to determine the relationship between WBI and health following experiences of weight stigma.36
Measurement of WBI and Health
To assess WBI, studies predominantly used the Weight Bias Internalization Scale (WBIS; n=53, 73.6%) or the Weight Self-Stigma Questionnaire (WSSQ; n=20, 27.0%). One study used the Weight Stigma Questionnaire (an older, one-factor version of the WSSQ), and two used the Acceptance and Action Questionnaire (AAQ) as a measure of WBI (e.g., with use of the weight-related self-stigma subscale).37,38 Of note, some studies used the AAQ scale or body image subscale as a process or outcome measure, rather than as the core measure of WBI.24,26,39
Overall, the WBIS and WSSQ showed good psychometric properties and validity. Both scales have been translated into several other languages, including Chinese, German, French, Italian, Iranian, Portugese, and Spanish. Modifications to the WBIS have been made in order to administer the scale to persons of varying weight statuses (WBIS – Modified),40 and both scales have been validated for use with youth.35,41–43 However, some inconsistencies were found with regards to item loadings. Several studies have dropped one or more items to improve the psychometric properties of the WBIS, thus creating variability in the literature with regards to how this scale is used and interpreted. With regards to the WSSQ, a total score was reported in some studies, whereas others reported separate scores for one or both of the subscales (Self-Devaluation and Fear of Enacted Stigma). In this review, we focused primarily on associations between health outcomes and the total WSSQ score; of the studies that did not provide a total score, we only included those that, at a minimum, reported outcomes associated with the Self-Devaluation subscale.
The vast majority of studies included at least one previously published and/or validated measure of health (versus a measure created for the study). Only 33.8% of studies reported that weight and height were measured objectively. A total of five studies included other objective measures of health, such as accelerometry data (to measure physical activity),25 blood pressure,24,44 blood glucose,44 cholesterol,29,44 heart rate,36 triglycerides,44 and waist circumference.29,44 Table 1 summarizes all selected studies of WBI and health in adults (excluding studies of youth and interventions to reduce WBI, which are discussed separately below).
Table 1.
Summary of published studies examining weight bias internalization (WBI) and health among adults
| Author (year, country, study design) | Sample Size and Type | Sample Characteristics (gender, race, mean age, mean BMI ± SD) | Measure of WBI | Measure(s) of Mental and/or Physical Health | Main Associations between WBI and Health |
|---|---|---|---|---|---|
| Almenara et al (2107; Canada; cross-sectional) | N=111; clinical - weight loss treatment | 100% women; race not reported (French Canadian); 40.9 years; mean BMI not reported (all BMIs ≥ 30 kg/m2) | WSSQ Self-Devaluation Subscale (French) | EDE-Q, FNAES, RSE | Lower self-esteem; higher fear of negative appearance evaluation, dietary restraint, and shape, weight, and eating concerns. |
| Baldofski et al (2016; Germany; cross-sectional) | N=240; clinical - prebariatric surgery | 68% women; race not reported (German); 45.1 years; 48.6±7.5 kg/m2 | WBIS-10 item version (German) | BMI, DEBQ, DERS, EAH, EDE-Q, YFAS | Higher levels of eating disorder symptoms, food addiction, emotional eating, and eating in the absence of hunger. No association with BMI. |
| Barber et al (2011; USA; cross-sectional) | N=70; clinical – patients with schizophrenia | 59% women; 57% black, 34% white, 7% Hispanic; 45.4 years; 36.8±7.0 kg/m2 | WBIS | BDI, MARS, Q-LES-Q-18 | Lower QOL and depression. Not associated with attitudes toward medication adherence or BMI. |
| Becker et al (2017; USA; cross-sectional) | N=503; community – food pantry patrons | 77% women; 11.3% white, 64.6% Hispanic, 16.5% black, mean age not reported (41.6% under age 50 years); BMI not reported | WSSQ | RCFIM | Higher in adults reporting household child hunger. |
| Boswell & White (2015; USA; cross-sectional) | N=664; online community | 88% women; race not reported; 37.7 years; 34.5±7.6 kg/m2 | WBIS | BDI, BMI, EDE-Q, QEWP-R | Higher BMI, depression, binge eating, and shape/weight concerns. In women only, greater purging, dietary restraint, and weight cycling. WBI more strongly associated with depression in women than men, and with binge eating in men than women. WBIS in women occurred at lower BMIs than men. |
| Burmeister & Carels (2014; USA; cross-sectional) | N=116; clinical – weight loss treatment | 74% women; 84.3% white, 6.1% Hispanic, 3.5% black, 3.5% Asian American; 43.5 years; 38.5±8.8 kg/m2 | WBIS | BES, BMI, CES-D, MBSRQ, SRHI, Television use | Greater binge eating and depression, and poorer body image. Not associated with BMI, television use, or physical activity. |
| Burmeister et al (2013; USA; cross-sectional and stepped care trial) | N=57; clinical – weight loss treatment | 68% women; race not reported; 47.4 years; 38.2 ±8.1 kg/m2 | WBIS | BES, BMI, CES-D, DEBQ, ESES, MBSRQ, OBCS-Shame, YFAS | Greater symptoms of food addiction, binge eating, depression, and body dissatisfaction; less eating self-efficacy. Not correlated with BMI or weight loss after 7 weeks. |
| Carels et al (2010; USA; RCT) | N=54; clinical – weight loss treatment | 81% women; 89% white; 47.4 years; 37.2±6.7 kg/m2 | WBIS | BES, BMI, CES-D, MBSRQ, weight loss | Greater binge eating, BMI, and appearance concerns. Not associated with depression or weight loss. WBI decreased significantly over time. |
| Carels et al (2013; USA; cross-sectional) | N=62; clinical – weight loss treatment | 79% women; 85% white; 43.7 years; 38.3±7.7 kg/m2 | WBIS | BES, BMI, CES-D, MBSRQ | Greater depression, binge eating, and body satisfaction. Not correlated with BMI. |
| Carels et al (2017; USA; stepped-care trial) | N=53; clinical – weight loss treatment | 87% women; 62% white, 34% black, 4% Asian/Pacific Islander; age not reported (>18 years); BMI not reported (≥27 kg/m2) | WBIS | Early weight loss success (i.e., need for stepped care), treatment drop-out | No difference in WBI among participants who needed to be stepped up once, twice, or not at all. No difference in WBI between participants who completed the program versus dropped out. |
| Douglas & Varnado-Sullivan (2017; USA: cross-sectional) | N=104; undergraduate students | 72% women; 70.2% white, 11.5% black, 12.5% other; 19.5 years; 26.1±6.8 kg/m2 | WBIS | DERS, EDDS | Greater disordered eating and emotion dysregulation. |
| Durso & Latner (2008; USA; cross-sectional) | N=198; online community | 83% women; 75.4% white, 14.7 black, 3.7% Hispanic, 30.5 years; 33.2±8.6 kg/m2 | WBIS | BMI, BSQ, DASS, EDDS, EDI, RSE | Initial development of the WBIS. Greater binge eating, depression, anxiety, drive for thinness, and body image concerns, and lower self-esteem. Not associated with BMI. |
| Durso et al (2012a; USA; cross-sectional) | N=100; clinical – BED treatment | 65% women; 79% white, 14% black, 4% Hispanic; 47.7 years; 40.6±6.6 kg/m2 | WBIS | BDI-II, BMI, EDE, RSE | Greater depression, disordered eating, shape/weight concerns, and lower self-esteem. Not associated with BMI or binge eating. |
| Durso et al (2012b; USA; cross-sectional) | N=486; online community | 81.7% women; 79.5% white, 5.3% Asian, 4.6% Hispanic, 39.1 years; 37.7± 13.2 kg/m2 | WBIS | EDDS, EDI-BD, EES | WBI mediated the relationship between perceived weight discrimination and eating disturbances (including binge frequency, emotional eating, body dissatisfaction, drive for thinness, and purging behaviors). |
| Durso et al (2016; USA; cross-sectional) | N=90; clinical – weight loss treatment | 64% women; 33% multi-racial, 24% white, 23% Asian, 10% Native Hawaiian/Pacific Islander; 49.7 years; 35.8±7.9 kg/m2 | WBIS-9 item version | BMI, BSQ, DASS, RSE | Greater depression and stress and lower self- and body-esteem. Not associated with anxiety or BMI. |
| Eisenberg et al (2017; USA; cross-sectional) | N=229; clinical – weight loss treatment | 100% women; 35% white, 65% black; 35.3 years; 35 ±7.7 kg/m2 | WBIS | Single item assessing family weight history | Lower WBI in white (but not black) women who reported a family weight history of overweight/obesity. |
| Essayli et al (2017; USA; experimental) | N=113; undergraduate students | 100% women; 45.1% Asian, 23% white, 16.8% mixed ethnicity; age not reported; BMI not reported (range 21.5–27.5 kg/m2) | WBIS-M | Weight labels, weight status | Assigning a weight label of “overweight” led to higher WBI, regardless of objective weight status. |
| Farhangi et al (2017; Iran; cross-sectional) | N=170; community health center | 100% women; Iranian; 31.3 years; 81.2% overweight, 17.1% obesity | WSSQ | GHQ-12, SF-12 | Lower mental and physical HRQOL. |
| Hain et al (2015; Germany; cross-sectional) | N=94; clinical endocrinology patients | 66% women; German nationality; age not reported (range 21–68 years); 45.4±7.6 kg/m2 | WSSQ (German) | BMI, BDI, FDS-20, GHQ-12, IWQOL, SF-12, WEB-SG | Greater depression, shame, guilt, and dissociative symptoms, and lower HRQOL. Not correlated with BMI, but higher among those with BMIs > 50. |
| Hilbert, Braehler et al (2014; German; cross-sectional) | N=1158; nationally-representative | 46% women; German nationality; 53.6 years; 80.4% overweight, 19.6% obesity | WBIS (German) | BMI, CSES, EQ-5D, Health Care Utilization Questionnaire, GAD-2, PHQ-2, VAS | Poorer self-evaluation and health status, and higher BMI, depression, and anxiety. Greater health care utilization when mediated by self-evaluation. BMI predicted higher WBI. Women had higher WBI and anxiety than men. |
| Hilbert, Baldofski et al (2014; Germany; cross-sectional) | N=1092; nationally-representative | 47% women; German nationality; 53.9 years; 28.3±3.7 kg/m2 | WBIS (German) | BDI-PC, SSS-8, weight status | Greater depressive symptoms, weight status, and severity of somatic symptoms (e.g., stomach aches). Higher WBI in adults with obesity than overweight. |
| Hilbert et al (2015; Germany; cross-sectional) | N=1158; nationally-representative | 46% women; German nationality; 53.6 years; 80.4% overweight 19.6% obesity | WBIS (German) | BMI, BDI-PC, EORTC-QLQ-C30, SCS, SSS-8 | Higher BMI and depressive and somatic symptoms. Lower self-compassion and QOL. |
| Himmelstein et al (2017; USA; cross-sectional) | N=956; national online subsample – experienced weight bias | 50% women; 64.7% white, 16.4% Hispanic, 13% black; 44.1 years; 26.7±5.7 kg/m2 | WBIS-M, 10-item version | BMI, items developed to assess coping with weight stigma | Higher BMI. Greater coping via avoidance (e.g., of physical activity) disordered eating, eating more, and negative emotions. |
| Hubner et al (2015; Germany; cross-sectional) | N=179; clinical - prebariatric surgery | 67.6% women; race not reported (German); 46.6 years; 48.7±7.3 kg/m2 | WBIS, 10-item version (German) | IPAQ-SF | Less physical activity. Mediated the relationship between general self-efficacy and moderate to vigorous physical activity. |
| Hubner et al (2016; Germany; cross-sectional) | N=78; clinical – prebariatric surgery | 55% women; race not reported (German); 41.7 years; 48.9±7.9 kg/m2 | WBIS and WSSQ (German) | BMI, GAD-7, IWQOL-Lite (total score and Self-Esteem subscale), MBSRQ, PHQ-9, | Greater appearance orientation, depression, and anxiety, and lower self-esteem and QOL. Neither associated with BMI. Larger effect size with WBIS vs. WSSQ. Scales correlated with each other. |
| Innamorati et al (2017; Italy; cross-sectional) | N=386; clinical –inpatient and outpatient obesity treatment | 85% women (inpatient), 66% women (outpatient); Italian nationality; 42.8 and 50.3 years; 29.8±4.9 and 44.8±8.3 kg/m2 | WBIS, 9-item version (Italian) | BES, BUT, CES-D, MMPI-2 LSE | Greater binge eating, depression, and body image-related concerns, avoidance, compulsive self-monitoring, and depersonalization. Lower self-esteem. |
| Jung et al (2017; Germany; cross-sectional) | N=878; nationally-representative | 44% women; German nationality; 56.4 years; 34.31±4.0 kg/m2 | WBIS (German) | MBSRQ-AS, weight discrepancy | Greater discrepancy between current and desired weight. Greater dissatisfaction with appearance. |
| Koball et al (2016; USA; cross-sectional) | N=242; community –medical visits not related to weight | 56% women; 98.7% white; 65.7 years; 31.1±9.5 kg/m2 | WBIS-M | BMI, GL-TEQ, MOS-GA | Higher BMI. WBI associated with trying to lose weight, reporting their doctor discussed weight, and weight loss. Less likely to adhere to weight loss recommendations from doctor. No association with physical activity. |
| Latner et al (2013; USA; cross-sectional) | N=120; clinical – weight loss treatment | 67.5% women; 30% white, 20% Asian, 39% mixed ethnicity; 48.3 years; 35.1±7.7 kg/m2 | WBIS | SF-12 | Poorer mental and physical HRQOL. |
| Latner et al (2014; USA; cross-sectional) | N=81; online community | 100% women; 97.5% white, 2.5%Asian; 41.1 years; 43.4±15.4 kg/m2 | WBIS | BMI, SF-36 | Not associated with BMI. Poorer mental and physical HRQOL. BMI moderated the effect of WBI on physical HRQOL. |
| Lee & Dedrick (2016; USA; cross-sectional) | N=243; undergraduate students | 100% women, 71% white, 23% Hispanic, 14% black; 22.6 years; 28.6 kg/m2 (range 18.7–60.7) | WBIS | BMI and self-perceived weight status | Acceptable fit of WBIS with one-factor solution when one item excluded. Good psychometric properties with BMI-based and self-perceived weight status. |
| Lent et al (2014; USA; longitudinal, observational) | N=170; clinical – bariatric surgery | 82% women; 89.5% white, 7.0% black, 2.0% Hispanic; 45.7 years; 47.8±8.3 kg/m2 | WBIS | BDI-II, percent weight loss | Greater depressive symptoms. Predicted lower percent weight loss 12 months post-operatively. |
| Lillis et al (2010; USA; cross-sectional) | N=169; community – online and prior weight loss treatment | 68% women; 69% white, 12% black, 8% Asian; 47 years; 31.7±6.6 kg/m2 | WSSQ | BMI, BSI, GHQ, ORWELL, TFEQ | Initial validation of the WSSQ. Good psychometric properties with 2 subscales (Fear of Enacted Stigma and Self-Devaluation). Higher BMI. Greater psychopathology, disinhibited eating, and hunger. Poorer HRQOL. |
| Lillis et al (2011; USA; cross-sectional) | N=87; clinical – weight loss treatment | 89% women; 91% white, 3% black, 5% Hispanic; 50 years; 33.1±7.3 kg/m2 | WSSQ | ORWELL | Poorer HRQOL. Mediated the relationship between BMI and HRQOL. |
| Lillis et al (2017; USA; open label trial) | N=188; clinical – online weight loss treatment | 76% women; 88% white; 55 years; 35.7±12.1 kg/m2 | WSSQ | BMI, EI, PROMIS Depression- and Anxiety-Short Forms, percent weight loss, treatment engagement | Greater anxiety, depression, disinhibited eating, dietary restraint. Fear of enacted stigma, but not self-devaluation, associated with higher BMI and less weight loss after 3 months. Participants high in weight self-devaluation viewed less online lessons. |
| Lin & Lee (2017; China; cross-sectional) | N=156; undergraduate students | 46% women; 100% Asian; 22.2 years; 27.4±3.2 kg/m2 | WSSQ (Chinese) | BMI, MBSRQ | Higher BMI. Poorer appearance evaluation and body satisfaction. |
| Magallares et al (2017; Spain; cross-sectional) | N=170; clinical – weight loss treatment | 35% women; race not reported (Spanish); 47.0 years; 42.8±8.3 kg/m2 | WSSQ (Spanish) | BMI, HADS | Higher BMI. Greater depression and anxiety. |
| Meadows et al (2017; UK; longitudinal) | Ns=658 and 614; undergraduate students and online community | 90% and 59.8% women; 76% and 58.6% white, 14% and 19.1% Asian, 3% and 5.2% black; 18.7 and 35.1 years; 22.0±3.9 and 27.9±8.7 kg/m2 | WSSQ | Yes/No item assessing food addiction; YFAS | More likely to have self-perceived food addiction in student but not community sample. |
| Mensinger & Meadows (2017; USA; RCT) | N=80; clinical – weight loss/neutral treatments | 100% women; 94% white; 39.6 years; 38.0±3.9 kg/m2 | WBIS | Red Lotus QOL Questionnaire (physical activity enjoyment and engagement) | Reductions associated with increased physical activity enjoyment, and mediated effects of intervention on physical activity engagement. Only participants with low WBI showed increased physical activity. |
| Mensinger et al (2016; USA; RCT) | N=80; clinical – weight loss/neutral treatments | 100% women; 94% white; 39.6 years; 38.0±3.9 kg/m2 | WBIS | EDE-Q, IES | Only participants with low WBI showed improvements in disordered and intuitive eating. Small reductions in WBI. |
| O’Brien et al (2016; Australia; cross-sectional) | N=634; undergraduate students | 73% women; 60% white, 37% Asian/Pacific Islander; 19.7 years; 22.4±4.1 kg/m2 | WBIS | BMI, DASS-21, LOCES-B, TFEQ-R18, | Higher BMI. Greater psychological distress, emotional eating, uncontrolled eating. Mediated the relationship between weight stigma experiences and disordered eating. |
| Palmeira et al (2016; Portugal; cross-sectional) | N=282; community | 100% women; race not reported (Portugese); 44.2 years; 31.4±4.5 kg/m2 | AAQW-R, WSSQ (Portugese) | BES, BMI, ORWELL | Higher BMI. Greater binge eating. Poorer obesity-related HRQOL. |
| Palmeira et al (2017b; Portgual; cross-sectional) | N=125; clinical – nutrition counseling | 100% women; race not reported (Portugese); 41.1 years; 34.4±5.5 kg/m2 | WSSQ (Portugese) | BES, BMI, FSCRS | Greater binge eating and worse self-image. Not associated with BMI. |
| Pearl & Dovidio (2015; USA; cross-sectional | N=237; online community - experienced weight bias | 44% women; 85.7% white, 4.6% black, 4.6% Hispanic; 34.2 years; 33.3±7.6 kg/m2 | WBIS-M | BMI, EDI-BD, scale created for exercise motivation/enjoyment | Higher BMI. Lower exercise motivation. Greater body dissatisfaction. No association with exercise intentions. |
| Pearl & Puhl (2014; USA; cross-sectional) | N=148; online community | 50% women; 79.1% white; 35.6 years; 27.9±7.3 kg/m2 | WBIS-M | BMI, self-perceived weight status, BSQ, DASS-21, EDDS, EDI- DFT, RSE | Higher BMI and BMI-based and self-perceived weight status. Greater body dissatisfaction, drive for thinness, depression, anxiety, and binge eating frequency. Lower self-esteem. Gender moderated effects of WBI on drive for thinness. |
| Pearl & Puhl (2016; USA; experimental) | N=260; online community | 48% women; 83.4% white, 7.3% black, 4.6% Hispanic; 34.6 years; 33.6±6.0 kg/m2 | WBIS | EDI-BD, PANAS-X, RSE | Increased negative emotion. Reduced self-esteem and positive emotion. Increased body dissatisfaction in men only. |
| Pearl et al (2017; USA; cross-sectional) | N=159; clinical – weight loss treatment | 88% women; 67.3% black, 22.6% white, 5.7% Hispanic; 43.8 years; 41.1±5.9 kg/m2 | WBIS | BMI, metabolic syndrome (triglycerides, HDL cholesterol, blood glucose, blood pressure, waist circumference), PHQ-9 | Greater depression and odds of meeting criteria for metabolic syndrome. Not associated with age, gender, or BMI. |
| Pearl et al (2015; USA; cross-sectional) | N=177; online community | 100% women; 80.8% white; 35.5 years; 32.8±6.9 kg/m2 | WBIS-M | BMI, GL-TEQ, SEES | Higher BMI. Lower exercise self-efficacy, motivation, and behavior. Did not moderate the relationship between experiences of weight stigma and exercise. Mediated the relationship between experiences and exercise. |
| Pearl et al (2014a; USA; cross-sectional) | N=245; clinical - BED and weight loss treatment | 70% women; 80.8% white; 48.0 years; 39.5±5.9 kg/m2 | WBIS | EDE, RSE | Greater overvaluation of weight/shape. Lower self-esteem. Overvaluation of weight/shape mediated relationship between self-esteem and WBI. |
| Pearl et al (2014b; USA; cross-sectional) | N=255; clinical -BED and weight loss treatment | 74% women; 80.8% white; 47.9 years; 39.3±6.0 kg/m2 | WBIS | BDI-II, BMI, EDE, SF-36 | Depressive symptoms mediated the relationship between WBI and mental and physical HRQOL. Not associated with BMI or BED symptom severity. |
| Puhl, Himmelstein et al (2017; USA; cross-sectional) | N=3504; national online panel, and weight advocacy group members | 56% women; 69.6% white, 12.4% Hispanic, 10.7% black; 44.0 years; 28.1±7.3 kg/m2 | WBIS-M, 10-item version | BMI, current attempts to lose/maintain weight, one item on dieting behavior, self-perceived weight status | Higher BMI and self-perceived weight status. More dieting and attempts to lose weight. Approximately 40% of US adults internalize weight bias, and 20% to a high degree. |
| Puhl, Quinn et al (2017; USA; cross-sectional) | N=549; national online panel of adults who had lost weight in past year | 59% women; 66.7%white, 11.3% black, 15.1% Hispanic; 42.2 years; 27.8±5.5 kg/m2 | WBIS-M, 10-item version | GL-TEQ, one item on eating breakfast, PSS-4, two items on dietary monitoring, self-perceived weight status, weight maintainer vs. regainer, WHO-QOL Scale-Brief | Lower physical activity, dietary monitoring, and physical HRQOL. Greater perceived stress. No association with eating breakfast. Higher self-perceived weight status. More likely to regain vs. maintain weight. |
| Puia et al (2017; Romania; cross-sectional) | N=99; clinical – gastroenterology outpatient center | 71% women; race not reported (Romanian); 48.0±14.7 years; 40.9±6.9 kg/m2 | WSSQ (Romanian) | Age of obesity onset; BMI; desire for bariatric surgery | Higher BMI and younger age of onset. No relationship to desire for bariatric surgery. |
| Raves et al (2016; USA; cross-sectional) | N=300; clinical – post-bariatric surgery | 96% men; race not reported (majority white); 53.7 years; 30.5±6.5 kg/m2 | WBIS, 8-item version | BMI, DEBS, FFQ-DA, percent BMI change (self-reported), PSA | Worse self-reported dietary adherence and greater disordered eating. Not associated with BMI or percent BMI change. |
| Schvey & White (2015; USA; cross-sectional) | N=197; online community, lean adults | 89% women; 77.2% white, 13.7% Asian, 4.1% other; 31.6 years; 22.3±1.9 kg/m2 | WBIS | BDI-II, BMI, EDE-Q, QEWP-R | Higher BMI. Greater depression, dietary restraint, eating/shape/weight concern, binge eating, and purging. |
| Schvey et al (2013; USA; cross-sectional) | N=656; online community | 85.7% women; 78.4% white, 7.9% black, 6.9% Hispanic; 37.6 years; 34.3±7.7 kg/m2 | WBIS | BDI-II, BMI, EDE-Q, QEWP-R | Higher BMI. Younger age of overweight onset. Greater depression, weight cycling, dietary restraint, and weight/shape/eating concern. Greater odds of having binge eating and purging. |
| Schvey et al (2016; USA; cross-sectional) | N=389; online community with gym memberships | 75% women; 53% white, 25% black, 11% Hispanic; 33.0 years; 35.6±7.7 kg/m2 | WBIS-M | BDI-II, BMI, current weight loss behaviors, Coping with Weight Stigma Questionnaire, SF-36, Stigma at the Gym Questionnaire | Higher BMI. Greater stigma at the gym and eating to cope with stigma. Poorer QOL. Not associated with depression or with healthy or unhealthy weight loss behaviors. |
| Sevincer et al (2017; Turkey; cross-sectional) | N=120; clinical – bariatric surgery | 80% women; race not reported (Turkish); 37.7±12.4 years; 46.1±6.1 kg/m2 | WSSQ (Turkish) | Alcohol consumption, BAI, BDI, BMI, DEBQ, EDE-Q, IWQOL-Lite, RSE | Higher BMI. Not associated with alcohol consumption. Greater anxiety, depression, binge eating, and eating/weight/shape concerns. Poorer self-esteem and quality of life. |
| Sienko et al (2016; USA; cross-sectional) | N=172; undergraduate students | 100% women; 70.3% white; 21.1 years; 29.7 kg/m2 (no SD provided) | WBIS | BMI, EDE-Q, PHQ-9 | Greater eating restraint, eating/weight/shape concerns, and depression. Mediated the relationship between depressive symptoms and disordered eating. Not associated with BMI. |
| Vartanian et al (2016; Australia; ecological momentary assessment) | N=46; community | 52% women; 45.7% white, 47.8% Asian; 28.4 years; 30.5 kg/m2 (range 22.3–42.6) | WBIS-M | BMI, resting heart rate, single items on physical activity, dieting, and motivation to lose weight | Higher resting heart rate. Lower motivation to exercise, diet, and lose weight following experiences of weight stigma. Not associated with BMI. |
| Wang et al (2017; USA; cross-sectional) | N=237; clinical - BED and weight loss treatment | 70% women; 77% white, 14% black; 47.9 years; 39.5±5.9 kg/m2 | WBIS | EDE, Ruminative Responses Scale, SCID for DSM-IV-TR | Greater rumination and overvaluation of shape and weight. |
| Webb & Hardin (2016; USA; cross-sectional) | N=333; undergraduate students | 100% women, 63% white, 20.2% black, 5.9% multi-racial/ethnic; 19.4 years; 23.5±4.9 kg/m2 | WBIS-M | BI-AAQ, BISS, BMI, IES-2 | Higher BMI. Lower self-compassion, body-related cognitive flexibility, and intuitive eating. Greater shame. |
| Weineland et al (2013; Sweden; cross-sectional) | N=178; clinical- post-bariatric surgery | 90% women, race not reported (Swedish); 41.5 years; 27.5±3.2 kg/m2 | Self-Stigma subscale of AAQ-W (Swedish) | BMI, BSQ, DASS, EDE-Q, EOQ | Higher BMI. Greater depression, anxiety, eating restraint, eating/shape/weight concerns, and emotional overeating. |
Note. SD = standard deviation. The term Hispanic is used for brevity and may also include persons of Latino/a and Mexican-American descent. When mean BMI was not reported in selected studies, weight statuses of participants were provided if available.
AAQ = Acceptance and Action Questionnaire (BI = Body Image, W-R = for Weight-Related Difficulties - Revised); BDI = Beck Depression Inventory (PC = Primary Care); BES = Binge Eating Scale; BISS = Body Image Shame Scale; BMI = Body mass index; BSI = Brief Symptoms Inventory; BSQ = Body Shape Questionnaire; BUT = Body Uneasiness Test; CES-D = Center for Epidemiological Studies Depression Scale; CSES = Core Self-Evaluation Scale; DASS = Depression Anxiety Stress Scales; DEBS = Disordered Eating after Bariatric Surgery; DEBQ = Dutch Eating Behavior Questionnaire (; DERS = Difficulty in Emotion Regulation Scale; EAH = Eating in the Absence of Hunger; EES = Emotional Eating Scale; EDDS = Eating Disorder Diagnostic Scale; EDE = Eating Disorder Examination (Q = Questionnaire); EDI = Eating Disorder Inventory (BD = body dissatisfaction, DFT = drive for thinness); EI = Eating Inventory; EORTC-QLQ-C30 = European Organisation for Research and Treatment of Cancer – Quality of Life Questionnaire; EOQ = Emotional Overeating Questionnaire; EQ-5D = EuroQol 5 Dimension; ESES = Eating Self-Efficacy Scale; FDS = Dissociative Experiences Scale (German); FFQ-DA = Food Frequency Questionnaire – Dietary Adherence; FNAES = Fear of Negative Appearance Evaluation Scale; FSCRS = Forms of Self-Criticizing/Attacking & Self-Reassuring Scale; GAD = Generalized Anxiety Disorder; GHQ = General Health Questionnaire; GL-TEQ = Godin Leisure-Time Exercise Questionnaire; HADS = Hospital Anxiety and Depression Scale; HRQOL = health-related quality of life; LOCES-B = Loss of Control of Eating Scale - Brief; IES = Intuitive Eating Scale; IPAQ-SF = International Physical Activity Questionnaire – Short-Form; IWQOL = MARS = Medication Adherence Report Scale; MBSRQ = Multidimensional Body Self Relations Questionnaire (AE = appearance evaluation; AS = appearance scale); MMPI-2-LSE = Minnesota Multiphasic Personality Inventory-2 Low Self-Esteem Content Scale; MOS-GA = Medical Outcomes Survey – General Adherence; OBCS = Objectified Body Consciousness Scale; ORWELL = Obesity-Related Well-Being Scale; PANAS-X = Positive Affect Negative Affect Schedule – Expanded version; PHQ = Patient Health Questionnaire; PROMIS = Patient Reported Outcomes Measurement Information System; PSA = Patient Dietary Success- Self-Assessed; PSS = Perceived Stress Scale; QEWP-R = Questionnaire for Eating and Weight Patterns – Revised; Q-LES-Q = Quality of Life Enjoyment and Life Satisfaction Questionnaire; RCFIM = Radimer Cornell Food Insecurity Measure; RSE = Rosenberg Self-Esteem Scale; SCID = Structured Clinical Interview for DSM; SCS = Self-Compassion Scale; SEES = Self-Efficacy to Exercise Scale; SF = Short Form Health Survey; SRHI = Self-Report Habit Index; SSS = Somatic Symptom Score; T1 and T2 = Time 1 and Time 2; TFEQ = Three-Factor Eating Questionnaire; VAS = Visual Analogue Scale; WBIS = Weight Bias Internalization Scale (M=Modified); WEB-SG = Weight and Body-Related Shame and Guilt; WHO-QOL = World Health Organization Quality of Life Scale; WSSQ = Weight Self-Stigma Questionnaire (WSQ = Weight Stigma Questionnaire); YFAS = Yale Food Addiction Scale; Scale.
Mental Health Outcomes in Adults
The emergence of research on WBI in recent years has included a considerable number of studies that examine links between WBI and mental health outcomes, of which findings suggest that WBI may be detrimental to a range of indices of psychological health. This literature is summarized below, focusing on associations between WBI and depression, anxiety, self-esteem, body image, eating disorder psychopathology, other psychological disorders and distress, and health-related quality of life (HRQOL).
Depression
Links between depressive symptoms and WBI have been examined in 30 studies.7,19,21,33,37,40,44–67 WBI was significantly and positively associated with depressive symptoms in 28 of the 30 studies; only two did not find a significant association.19,50 Bivariate correlations ranged from r=0.24 to r=0.66, with 25 studies reporting moderate (r≥0.30) or strong correlations (r≥0.50). Only one study compared links between depression and two different measures of WBI; among preoperative bariatric patients, both the WBIS and WSSQ were significantly associated with depression, with medium-sized effects for the WSSQ (β=0.43, p< 0.01) and larger effects for the WBIS (β=0.52, p<0.001).62
Correlations between WBI and depressive symptoms were present across both community and treatment seeking samples, and among individuals of different body weight categories. It is noteworthy that strong correlations were observed in both lean adults without overweight49 and among individuals with obesity,58,59 suggesting that WBI is present and associated with emotional distress for individuals across diverse body sizes. Importantly, WBI remained significantly associated with depressive symptoms after controlling for BMI,40,49,52,55 and some studies found no relationship between BMI and depression.54,56,60,64 Given other evidence that WBI is associated with having a higher BMI (described in more detail below), these findings suggest a distinction between WBI and depression. While studies generally documented links between WBI and depression for both women and men, several studies observed stronger correlations between these variables for women compared to men,45,46 although other work found that gender did not moderate this relationship.40 However, few of the 30 studies examined gender differences, and more research is needed to determine whether links between WBI and emotional distress differ for women and men.
Anxiety
Eleven studies examining psychosocial correlates of WBI have assessed anxiety.7,21,37,40,54,55,61–64,67 WBI was significantly and positively correlated with symptoms of anxiety in 10 studies; one study of adults enrolled in a behavioral weight loss program did not find a significant association between WBI and anxiety (measured with the DASS anxiety subscale), despite significant correlations observed between WBI and DASS subscales of depressive symptoms and stress.54 In the remaining 10 studies reporting significant associations, bivariate correlations were weak to moderate, with r values ranging from 0.23 to 0.55. Stronger correlations were typically observed when anxiety was measured with the DASS compared to other scales. As with depression, significant correlations between anxiety and WBI were observed in adults of varying weight statuses. In addition, correlations observed between WBI and anxiety have been documented in both community and clinical samples. Importantly, several studies found that WBI predicted anxiety over and beyond the variance accounted for by participants’ BMI.7,40 Of note, half of the current studies examining links between WBI and anxiety were conducted outside of North America, in Australia,55 Germany,61,62 Spain,64 Sweden,37 and Turkey.67
Self-Esteem
Self-esteem has been assessed as a correlate of WBI in 11 studies.7,32,40,51,54,59,61,67–70 Across all 11 studies, WBI was significantly correlated with self-esteem, indicating that higher internalization of weight bias is related to lower self-esteem. Bivariate correlations were moderate to strong (r values ranged from −0.40 to −0.68) in both community and clinical samples of adults with overweight and obesity. WBI was also found to be a significant and independent predictor of self-esteem, over and above BMI.7,40,54 One recent experimental study of 260 women with overweight or obesity demonstrated that self-directed stigma following a hypothetical weight-stigmatizing situation led to lower self-esteem, regardless of BMI.32
Some research has examined the mediating role of self-esteem in the relationship between WBI and other health indices. For example, a national German study of 1,158 adults found that core self-evaluation fully mediated the relationship between WBI and depression and anxiety (both large effects).61 These meditational analyses suggest that self-esteem may be a mechanism by which WBI could impair other health outcomes.
Body Image
To date, 27 studies have examined the relationship between body image and WBI.7,19,22,25,32,37,39,40,46,49,51,53,54,56–60,62,65–69,71–74 Across studies, body dissatisfaction and body image concerns were consistently and significantly correlated with WBI, indicating that higher levels of WBI were associated with worse body image and increased body dissatisfaction. Of the studies that provided correlations (n=18), 16 reported strong correlations (r values=0.51–0.80), and only two studies reported a correlation below r=0.30.62,67
Similar to correlational findings for WBI and depression, the current literature shows that links between WBI and poor body image are present, and strong, for individuals of diverse body sizes. Furthermore, the consistency and strength of these associations are present in clinical samples of adults seeking treatment for weight loss,54,58,59 BED,51,69 or bariatric surgery,37,67 as well as community samples.7,40,46,66 Importantly, the relationship between WBI and body image remains significant even after controlling for variables such as BMI,7,40,46,66 depression,46,51,66 and other psychological measures.51 Studies examining the effects of gender (n=4) did not find significant differences in correlations between WBI and body image,40,46,54,69 despite higher levels of WBI in women versus men. As an example, in a community sample of adults with overweight and obesity (N=148), WBI was a significant predictor of body image, and gender did not moderate these results.40
Disordered eating
Disordered eating has emerged as a common focus of recent literature in the context of WBI. Collectively, 31 studies have examined links between WBI and different aspects of disordered eating, including binge eating (n=18), other eating disorder pathology or non-normative eating behaviors (n=22), and symptoms of food addiction (n=3). Consistently, this literature shows significant and positive associations between WBI and symptoms of eating disorder pathology.
Binge eating
Moderate to strong correlations were consistently reported between WBI and binge eating symptoms (r values=0.43–0.62).7,19,38,40,46,48,49,51,56–59,65,69,70,73,75 Only one study reported a correlation of less than r=0.30.67 These associations were documented in both community and clinical samples.19,56–59,66,67,70,75 Significant correlations were also reported for links between WBI and frequency of binge eating in the past 3 or 6 months, as well as objective and subjective binge eating episodes (r values=0.25–0.53).7,40,46 Two studies of treatment-seeking samples of individuals with obesity and BED did not find significant associations between WBI and BED symptom severity,48,51 though this may be a result of more frequent binge eating in BED samples compared to community or other types of clinical samples.
Importantly, associations between WBI and binge eating remained significant after controlling for BMI and other weight and eating-related psychosocial and behavioral variables.7,40,56,66 While most literature to date has examined these links among individuals with higher body weight, research with non-overweight adults has similarly documented strong associations. For example, in a study of 197 lean adults, Schvey and White49 found that participants with higher WBIS scores had over two times greater odds of meeting binge eating criteria. These findings persisted after controlling for depression and BMI. Although few studies have assessed gender differences, some work has demonstrated associations between WBI and binge eating in both men and women.46
Other eating pathology
Studies examining links between WBI and eating disorder pathology (such as dietary restraint, drive for thinness, emotional eating, purging, or other maladaptive eating behaviors) have been examined using a variety of validated measures.7,21,22,34,37,40,46,49,51,55,57,60,63,66–68,73,75–77 or survey items created by researchers to assess eating behaviors specifically in response to experiences of weight stigma.50,78 Across these measures, studies have demonstrated significant correlations between WBI and dietary restraint (r values=0.21–0.50), eating concerns (r values=0.37–0.64), drive for thinness (r=0.47), as well as measures assessing disinhibition, uncontrolled eating, and emotional eating (r values=0.46–0.65). Moderate to strong correlations (r values=0.29–0.77) were documented for associations between WBI and global or total scores for measures of disordered eating.37,46,49,51,57,60,63,67,77 As with binge eating, measures of eating pathology were associated with WBI in both clinical and community samples and across body weight statuses. In addition, WBI has been found to predict eating psychopathology (including purging behaviors), above and beyond measures of depression and self-esteem.51,66
Several noteworthy findings have emerged in this literature that provide initial insights on the relationship between WBI and eating disorder psychopathology. Two studies have found that WBI mediates the relationship between the experience of being stigmatized due to one’s weight and disordered eating. In a community sample of 228 adults with overweight and obesity, Durso et al73 tested the impact of WBIS scores on the relationship between perceived weight discrimination and eating pathology (including binge eating, emotional eating, bulimic symptoms, and drive for thinness) and found that WBI mediated this relationship even after controlling for BMI. O’Brien et al55 found similar results in a sample of 634 undergraduate students, where the relationship between weight stigma experiences and emotional and uncontrolled eating was mediated by WBI. Specifically, participants who reported having experienced weight stigma had greater WBI, which was associated with more psychological distress, which was in turn associated with more maladaptive eating behaviors. These findings align with recent evidence from a nationally-representative US sample, which found that individuals with higher WBI were more likely to report coping with experiences of weight stigma by eating.78
Food addiction
Three studies to date have examined WBI in the context of symptoms of food addiction.34,57,76 These studies have demonstrated significant correlations between WBI and greater food addiction symptoms, as measured by the Yale Food Addiction Scale (YFAS). For example, a recent German study of 240 pre-bariatric patients found that WBI was associated with higher levels of food addiction and eating disorder pathology with medium-to-large effects (p values<0.01).76
Other psychological disorders and distress
Eleven studies have examined the relationship between WBI and other indices of psychological distress, including emotion regulation75,76 (such as rumination65), perceived stress,79 negative affect,32 dissociative experiences,53 somatic symptoms,47,52 maladaptive coping with experiences of weight stigma,78 and general psychological distress.63,80 Collectively, this research found that WBI was consistently and significantly associated with increased psychological distress. Moderate correlations were observed between WBI and brooding rumination, emotion dysregulation, dissociative experiences, and perceived stress. Weaker correlations were observed for somatic symptoms, although Hilbert et al52 showed that WBI independently contributed to somatoform symptoms over and above BMI in a community sample (N=1,092). Experimental research has also demonstrated a significant effect of WBI on affect, leading to greater negative affect (F=7.92, p<0.01) and less positive affect (F=4.11, p<0.05) than the experience of weight stigma from others in an online sample of adults with overweight and obesity (N=260), regardless of BMI.32 These findings suggest that WBI may be a stronger predictor of psychological distress than experiences of weight stigma alone.
HRQOL
Fifteen studies have examined and demonstrated significant correlations between WBI and both general and weight-specific HRQOL.38,45,47,48,50,53,61–63,67,79–83 Some of the measures used included subscales that distinctly assess mental versus physical QOL (e.g., Short Form [SF]-12, SF-36, Impact of Weight on Quality of Life [IWQOL]), while others only include one composite score (e.g., Obesity-Related Well Being Scale [ORWELL]).
Mental HRQOL
Six studies have examined associations between WBI and mental HRQOL using the Mental Component Summary Score (MCS) of the SF-12 or SF-36.48,50,53,80–82 Across these studies, WBI was significantly and negatively associated with mental domains of quality of life, and these findings remained consistent for both the WBIS and WSSQ. An additional study found that both the WSSQ and WBIS were associated with poorer mental HRQOL using the self-esteem subscale of the IWQOL.62
Six studies have examined and demonstrated significant correlations between WBI and weight-specific quality of life using the IWQOL and ORWELL (r values=−0.28 to −0.69).38,53,62,63,67,83 While these associations have been observed for both the WSSQ and WBIS, Hubner et al62 who compared these measures in a sample of 78 pre-bariatric patients found stronger associations with the IWQOL when WBI was measured using the WBIS (β=0.57, R2=0.33, p<0.001) compared to the WSSQ (β=0.45, R2=0.20, p<0.001).
Several studies have reported mediational analyses examining the relationship between self-stigma and weight-related QOL. For example, in a sample of 87 treatment-seeking adults with overweight and obesity, Lillis et al83 found that self-stigma mediated the relationship between BMI and obesity-related quality of life. Pearl et al48 found that, among patients with obesity and BED (N=255), depression mediated the relationship between WBI and HRQOL, as measured by the SF-36. Taken together, the existing literature suggests that WBI may be detrimental for mental HRQOL. Of note, all studies were cross-sectional, thus limiting conclusions about directionality and causality.
Physical HRQOL
Seven studies consistently showed significant associations between WBIS scores and physical HRQOL.47,48,50,61,79,81,82 For example, Latner et al81 found that, among 120 treatment-seeking adults with overweight/obesity, WBIS scores predicted the physical component score (PCS) of the SF-36, even after controlling for BMI, age, exercise, medical conditions, and medication use. In another study by Latner et al,82 WBIS scores moderated the relationship between BMI and PCS scores in women with obesity (N=81), such that women with higher BMIs only had worse physical HRQOL when they also had higher (but not lower) WBIS scores. Notably, this study did not show any effects of perceived weight discrimination on physical HRQOL, highlighting the unique contribution of WBI. More work is needed to clarify additional mechanisms in the relationship between WBI and self-perceived health.
The relationship between physical HRQOL and WBI as measured by the WSSQ is less clear. Farhangi et al80 found a significant association between the WSSQ total score and the PCS of the SF-36, but did not find an association between the self-devaluation subscale and this scale. Hain et al.53 also did not find a significant correlation between the WSSQ total score and SF-36 PCS. However, Sevincer et al67 reported a significant correlation between the WSSQ total score and the physical function subscale of the IWQOL. Hain et al53 and other researchers have also found significant associations between the WSSQ and weight-specific QOL scales, such as the IWQOL total score and the ORWELL.38,53,63,83 Both of these scales combine mental and physical HRQOL into one score, so we cannot determine their relative associations.
Physical Health Outcomes in Adults
In comparison to studies of mental health outcomes, less research has assessed the relationship between WBI and physical health, and findings are less consistent. Studies on physical health have mostly focused on the relationship between WBI and weight (including BMI, weight loss, and weight regain) or weight-related health behaviors (e.g., dietary adherence and physical activity). Studies examining other health outcomes (e.g., cardiometabolic risk and treatment adherence) are also reviewed below.
Body weight
BMI
Forty-two cross-sectional studies examined the relationship between WBI and BMI or categorical weight status (i.e., normal weight, overweight, and obesity). Among samples that only included persons with overweight/obesity, 16 studies found significant associations between WBI and BMI or weight status,10,19,37,38,46,47,50,52,53,61,63,64,66,67,72,74,79,84,85 and 17 found no significant associations.7,21,36,44,45,48,51,54,56–58,60–62,70,76,77,82 In studies that found significant associations, r values ranged from 0.12 to 0.40. One study found no significant linear relationship between BMI and WSSQ scores (r=0.14, p=0.18), but did find that patients with BMIs ≥50kg/m had significantly higher scores than those with BMIs of 35–49.9kg/m2 (p=0.017).53 Among the nine studies that also included participants with lower body weights (i.e., BMIs < 25kg/m2), all found significant associations between BMI and WBI.10,37,39,40,49,55,72,78,79,86 Thus, although the literature does not show a consistent, linear relationship between body weight and WBI among persons who have higher body weight, higher weight appears to be associated with higher WBI when a broad range of body weights are represented.
Three of these studies also found significant associations between WBI and higher self-perceived weight status, independent of objective weight status as measured by BMI.10,40,79 In two of these studies,10,40 self-perceived weight status was more strongly associated with WBI than was objective weight status. Lee and Dedrick87 showed that the WBIS retained its psychometric properties regardless of whether it was administered to participants with a self-perceived versus objective weight status of overweight/obesity, and scores were higher when weight status was defined by self-perceptions. Furthermore, in an experimental study of undergraduate women with BMIs of 21.5–27.5, women who were “labeled” as overweight as part of the study manipulation had higher WBIS scores than those labeled as normal weight, regardless of their objective weight category.31 Taken together, these findings suggest that researchers can expand their criteria when defining “overweight,” since WBI may affect individuals who do not meet objective weight classifications.
Weight loss
Six studies have assessed the relationship between WBI and weight loss following behavioral (n=4)19–21,57 or surgical (n=2)33,77 treatments. None of the behavioral weight loss studies found associations between WBI (assessed with the WBIS and Self-Devaluation subscale of the WSSQ) and weight loss following short-term (7–14 weeks) treatment. Among the two studies assessing effects of WBI on weight loss via bariatric surgery, Raves et al77 found no association between WBI and percent weight change after surgery, while Lent et al33 found that higher baseline WBIS scores predicted less percent weight loss at 12 months after controlling for demographics, baseline BMI, depression, and surgery type (p=0.04). Of note, Raves et al77 did not standardize the time since surgery, and pre and post weight were assessed via self-report.
Aside from measuring weight loss, three studies have assessed self-reported weight loss attempts and motivation. Vartanian et al36 found that, following acute instances of weight-stigmatizing experiences, WBI was associated with less motivation to lose weight among adults with overweight/obesity (p=0.04). Puhl et al10 found that, among over 3500 adults, those who reported trying to lose weight in the past year had higher WBIS-M scores (β=.08, p<0.001). Koball et al86 also found that, among 242 patients seeking non-weight-related medical care, those with higher WBI were more likely to report trying to lose weight (p<0.001). Thus, this initial evidence suggests that WBI may be associated with greater efforts to lose weight, but perhaps not immediately following instances of weight-based stigmatization.
Weight regain vs. maintenance
Two studies have assessed WBI in relation to weight cycling, defined as losing and regaining 20 lb or more.46,66 Results showed that WBIS scores correlated with greater frequency of weight cycling (r values=0.19 to 0.20), although one study only found this association among women but not men.46 Additionally, in a self-report study of 549 adults who reported losing at least 10% of their body weight in the past year, Puhl et al79 found that adults who had regained at least 5% of their weight had higher WBIS-M scores than those who maintained their weight loss (4.6 vs. 3.5, p<0.001). Logistic regression analyses showed that higher WBIS-M scores were associated with lower odds of maintaining lost weight (odds ratio=0.72, p<0.001), even after controlling for engagement in maintenance behaviors, stress, BMI, and demographics. Thus, while evidence examining the relationship between WBI and initial weight loss are mixed, these two studies show consistent negative effects of WBI on weight loss maintenance.
Eating behaviors related to weight management
Ten studies have assessed the relationship between WBI and eating behaviors and experiences pertinent to weight management, including: reported hunger;63 the ability to respond to hunger and satiety cues (i.e., intuitive eating);22,39 self-monitoring behaviors,79 eating to cope with stigma;78 self-efficacy to avoid overeating;57 adherence to the postsurgical diet following bariatric surgery;77 and efforts to eat healthfully and diet.10,36,50
Findings regarding the relationship between WBI and dieting are mixed. For example, Puhl, et al10 found that, among adults who had lost at least 10% of their body weight in the past year, those with high levels of WBI were more likely to report dieting in the past year than those with low levels of WBI (71.7 vs 94.9%, p<0.001). Dieting in the past year remained a significant predictor of WBI in linear regression analyses that controlled for variables such as BMI, experiences of weight stigma, and demographics. In contrast, Vartanian et al36 found that higher WBIS scores were associated with lower motivation to diet in response to acute reports of weight stigmatization (p=0.03). The vague use of the term “dieting” may explain these mixed findings, as people may attempt to diet in both healthy (e.g., reducing portion sizes) and unhealthy (e.g., skipping meals) ways. Additionally, as illustrated by Himmelstein et al,78 some people respond to instances of weight stigma with urges to eat more food (thus the opposite of dieting). Schvey et al50 reported an association between WBIS scores and maladaptive coping strategies in response to weight stigma (r=0.59, p< 0.01), which included both eating more food and using extreme dieting behaviors to lose weight quickly. Of note, Schvey et al50 did not find an association between WBIS scores and more general reported engagement in healthy or unhealthy weight loss behaviors.
Aside from dieting, four studies have documented a consistent, negative relationship between WBI and other weight management-related eating behaviors. In a study of 300 adults who had undergone bariatric surgery,77 small but significant associations were found between WBI and worse adherence to the postoperative diet, as assessed by patients’ self-evaluation (i.e., how well they thought they were adhering to the diet; r=−0.19) and by an adapted version of the Food Frequency Questionnaire (r=−0.18, p values<0.01). Another study of 549 adults who had recently lost weight found an association between WBIS-M scores and reported frequency of dietary monitoring (r=−0.14, p<0.05), which is a strong predictor of successful weight management. Additionally, Burmeister et al57 found a strong, negative correlation (r=.46, p<.01) between WBIS scores and self-efficacy to control urges to overeat among 57 adults with overweight/obesity seeking BWL treatment. Finally, Mensinger et al22 found that WBI moderated the effects of lifestyle intervention on improvements in intuitive (or adaptive) eating behaviors. Participants high in WBI did not show improvements in intuitive eating, while those low in WBI did. Together, these findings suggest that, while the evidence of an association between WBI and dieting is mixed, WBI appears to have negative associations with eating-related behaviors and psychological factors that promote successful weight management.
Physical activity
Ten studies tested associations between WBI and physical activity.23,36,50,56,74,78,79,84,86,88 Seven of these studies measured self-reported engagement in physical activity (e.g., minutes of moderate-to-vigorous activity), and six included measures of exercise-related motivational factors (e.g., self-efficacy). Physical activity measures included validated self-report questionnaires,56,79,84,86,88 single-item assessments,23,36,78 and self-report scales created specifically for the studies.50,74,79
Studies did not consistently find a direct relationship between WBI and engagement in physical activity. Four studies found small, marginally or statistically significant effect sizes for the association between WBIS scores and reported engagement in physical activity, with r and beta (β) values ranging from −0.14 to −0.22.56,79,84,88 One study found no association between WBIS-M and frequency of exercising at various intensities86 and another found that WBIS-M scores were not associated with the frequency of going to the gym.50 However, three studies did show WBI to be a significant mediator or moderator of physical activity. For example, in a study of women with obesity receiving a lifestyle intervention, Mensinger and Meadows23 found that those with high WBI did not show significant increases in physical activity, while those low in WBI did. They also found that WBIS scores mediated the effects of the intervention on increased physical activity. Pearl et al84 showed that WBI did not moderate the effects of experiencing weight stigma on physical activity for women with overweight/obesity, but it did mediate this relationship. Thus, while a direct relationship between WBI and physical activity remains unclear, WBI may determine how other experiences and interventions affect physical activity.
Associations between WBI and motivational factors related to physical activity – such as exercise self-efficacy, enjoyment, and avoidance – appear to be stronger and more consistent than associations between WBI and physical activity engagement.23,36,50,74,84 In a large, US national sample, adults with higher WBIS-M scores reported higher scores on a scale assessing avoidance of physical activity as a coping response to weight stigma.78 Schvey et al50 created a self-report measure containing three subscales related to exercising at the gym for people with obesity: stigma at the gym, self-consciousness at the gym, and negative attitudes toward the gym. Significant correlations were observed between all subscales and WBIS-M scores (r values ranging from 0.19 to 0.41), as well as correlations between WBI and two subscales assessing perceived barriers to exercise. Additionally, Vartanian et al.36 found that higher WBI was associated with less motivation to exercise following experiences of weight stigma. Thus, studies consistently show associations between WBI and reduced self-reported motivation to exercise.
Cardiometabolic risk
To date, only two studies have examined the relationship between WBI and cardiometabolic risk factors. In a community sample of 46 adults, Vartanian et al36 found a correlation between WBIS scores and resting heart rate (r=0.31, p<.05). Pearl et al44 assessed WBI and criteria for metabolic syndrome in 159 treatment-seeking adults with obesity. Results showed that, when controlling for demographics, BMI, and depressive symptoms, WBIS scores were marginally (p=0.052) associated with increased odds of having metabolic syndrome. However, when WBIS scores were divided into tertiles, participants with high levels of WBI had three times greater odds of having metabolic syndrome than those with low levels of WBI. Additionally, WBIS scores were significantly and positively associated with triglycerides when controlling for all covariates, regardless of whether WBIS scores were analyzed continuously or categorically. These findings require replication but suggest a link between WBI and poorer cardiometabolic health.
Other health behaviors and outcomes
Four studies assessed adherence to treatments related and unrelated to weight. One study of 70 patients with schizophrenia enrolled in a weight loss study found no relationship between WBIS scores and attitudes toward antipsychotic medication adherence,45 suggesting that WBI does not necessarily translate to reduced self-efficacy and motivation to engage in non-weight-related behaviors. With regards to weight loss, two studies found reduced treatment adherence among adults with higher levels of WBI, as measured by adherence to their doctor’s weight loss recommendations86 and number of sessions attended in an online weight loss program.21 Another study found no difference in WBI between participants who completed a weight loss program and those who dropped out.20
Seven studies have examined the relationship between WBI and other outcomes related to weight and health. These studies reported the following findings: WBI is lower among white adults with (versus without) a family weight history of overweight/obesity;89 higher WBI is associated with a younger age of onset of overweight/obesity66,85 and reports of food insecurity;90 and WBI is not significantly related to television use,56 health care utilization,61 or alcohol consumption.67
Studies of WBI in Youth
Two studies have validated the WBIS in adolescents: one in a sample of 57 US adolescents seeking bariatric surgery43 and one among 191 German adolescents seeking treatment for overweight/obesity.41 Between the two studies, and controlling for BMI, WBIS scores correlated with: depressive symptoms; anxiety; psychiatric problems by both child and parent report; self-esteem, disordered eating symptoms, including frequency of objective binge eating episodes; body image concerns; general self-efficacy; and HRQOL (absolute r values = 0.28 to 0.81). However, in one study, WBIS scores was not associated with the presence of psychiatric diagnoses, psychiatric treatment, or suicidal ideation as determined by clinical interview.43 Semi-structured interviews by Ciupath-Plath et al41 confirmed the acceptability and accessibility of scale. Thus, the WBIS appears to be valid for use in adolescents. Additionally, one study validated the WSSQ in a sample of 156 French-speaking, Canadian adolescents with overweight/obesity.42 This study found support for a two-factor solution and significant associations between the self-devaluation subscale and self-esteem, body image, disordered eating, depression, and anxiety (absolute r values = 0.24 to 0.43), though not BMI.
Only one prospective study has assessed WBI in children (ages 7–11). Zuba & Warschburger35 conducted a 2-year longitudinal study of over 1000 German children, making minor changes to the WBIS item wording to be appropriate for children of all weight statuses. Results showed that children with overweight scored higher on the WBIS than non-overweight children, although at Time 1, BMI correlated with the WBIS more strongly among non-overweight than overweight children. No gender differences were found for correlations between WBIS and BMI, restrained eating, emotional eating, or conduct problems (r values = 0.10 to 0.46). Higher BMI at Time 1 predicted higher WBIS scores two years later for non-overweight (but not overweight) boys and girls. Furthermore, WBIS scores at Time 2 mediated the relationship between BMI at Time 1 and emotional problems (in non-overweight children) and restrained eating (for both weight statuses) at Time 2. Thus, findings from this single study suggest that adverse associations with WBI may begin during youth.
Interventions to Reduce WBI
Seven studies have tested the effects of psychological interventions, often combined with healthy eating or weight loss programs, on reductions in WBI. Five of these studies have tested interventions based on Acceptance and Commitment Therapy (ACT), which focused on topics such as self-compassion, mindfulness, and “experiential avoidance” (i.e., the tendency for people to avoid uncomfortable feelings).24,26–29 Only one study was a randomized controlled trial, which tested the effects of the “Kg (kilogram)-free” program (ACT combined with a healthy eating program) compared to treatment as usual (TAU; medical and nutritional visits) in 73 women with overweight/obesity.29 Results showed that, after 12 sessions, participants in the KG-free intervention had significantly greater improvements in WBI, psychiatric symptoms, HRQOL, physical activity, and disordered eating than participants who received TAU (d values ranged from 0.44 to 0.85). The intervention also conferred small but significant benefits for reduction in BMI compared to TAU (d = 0.09), but did not affect cardiometabolic risk factors such as waist circumference or cholesterol. Other smaller studies without control groups have found similar benefits for mental health, HRQOL, and health behaviors up to 3 months following treatment.24,26–28
One study has tested the effects of an intervention for WBI adapted from cognitive-behavioral therapy, without any weight loss or health behavior intervention.30 Results showed significantly greater improvements in WBIS scores, stereotype endorsement, and weight self-efficacy among participants who attended the 8-week intervention program, compared to those in the quasi-control group who did not receive any intervention ( values = 0.36 to 0.39). There were no significant differences in weight change between the two groups, signifying that these improvements were attributable to the psychological intervention rather than changes in weight.
Additionally, Carels et al25 tested a weight loss intervention that included some content on WBI (using similar cognitive-behavioral strategies as those described above), in comparison to a standard behavioral weight loss (BWL) program. Results showed that WBI decreased in both groups, and no differences were found between groups for outcomes such as binge eating, body satisfaction, and weight loss. Due to a number of differences between the two programs apart from the inclusion of a stigma intervention, it is difficult to decipher the effects of the stigma intervention specifically. Of note, only two studies have explored the effects on WBI of weight loss and healthy eating programs, without specific interventions targeting WBI.19,22 These studies have generally found small but significant decreases in WBI (e.g., ½ point on the 7-point WBIS). The magnitude of these WBI reductions are smaller to those found in the aforementioned stigma intervention studies (e.g., 1 point on the WBIS30).
Discussion
This systematic review provides a synthesis of the evidence linking WBI to mental and physical health outcomes. Although largely an understudied topic, WBI has gained increasing empirical attention in the past decade, and particularly in the past 1–2 years. Overall, evidence summarized in this review shows that WBI is consistently associated with negative mental health outcomes such as depression, anxiety, poor self-esteem and body image, disordered eating, and impaired mental HRQOL. Studies assessing the association between WBI and physical health were fewer and less consistent in their findings. However, clear associations have been demonstrated between WBI and higher severity of obesity, reduced motivation/self-efficacy to engage in health-promoting behaviors (e.g., physical activity), and impaired dietary adherence.
A notable finding from the current review is the overwhelming use of two self-report scales – the WBIS and WSSQ (and iterations, such as the WBIS-M) - to assess WBI. Although validated in a number of studies that included translated versions, the psychometric properties of the WBIS have been somewhat inconsistent, with some studies finding 1 or 2 factor solutions that included all 11 items or excluded 1 or 2 items. Additional consideration is also warranted to determine whether the items included in the WBIS and WSSQ truly capture the internalization of negative weight stereotypes and self-derogation due to weight. For example, the Fear of Enacted Stigma subscale of the WSSQ assesses anticipated stigma from others, which has been differentiated from internalized stigma in prior work.91 Only one study to date has compared the WBIS and WSSQ, and no clinical cutoffs for either scale have been established. Efforts to improve measurement of this important construct are needed. This may include the development of new measures that clearly assess key aspects of internalization, including (1) awareness of one’s stigmatized identity, (2) agreement with weight-based stereotypes, (3) application of these stereotypes to oneself, and (4) self-devaluation based on this stigmatized identity. Improvements in measurement will enhance the quality of future studies and more accurately assess the effects of WBI on health. Greater standardization of the measurement of WBI (as well as its related health outcomes) will also allow for better synthesis of key findings, such as through meta-analysis.
Strengths of prior research include assessment of WBI and health across the spectrum of body weight statuses and in both clinical and community samples. Significant findings in these studies highlight the broad impact of WBI, regardless of one’s objective weight status or efforts to seek treatment for obesity. However, several considerable limitations of the current body of existing evidence that must be addressed in future research to advance our understanding of the effects of WBI on health.
First, the vast majority of studies to date have relied solely on self-reported measures of health. Subjective distress is an important outcome to assess, as it reflects the individual’s psychological experience. Still, more objective measures of health should be included in future studies, such as: psychiatric diagnoses as assessed by clinician interview/rating; accelerometry data to track physical activity; cardiometabolic risk factors such as blood pressure, waist circumference, blood glucose, cholesterol, triglycerides, and other biological markers of health; and obesity-related comorbidities as defined by diagnoses of diabetes, hypertension, sleep apnea, etc. Objective assessments would help to clarify discrepancies in self-reported health outcomes (e.g., eating more or less in response to WBI) and enhance confidence in study findings by reducing bias and corroborating self-report measures.
Another major limitation is the lack of gender and racial/ethnic diversity in the majority of studies. The predominant focus on white women (versus men or women of color) limits the generalizability of prior findings. Because existing measures of WBI were developed primarily in white, female samples, these measures also may not adequately capture the experiences of other populations. Future research should include more diverse samples in both scale development and assessments of WBI as it relates to health, as well as in intervention studies to reduce WBI. Additionally, other forms of diversity (such as sexual orientation) have been neglected in this area of research and should be considered in future work. Further assessment and adaptation of WBI measures in children and adolescents are also needed to understand the developmental effects of WBI on health across the lifespan.
Finally, prior research assessing WBI and health has been predominantly cross-sectional in nature, with only one study experimentally testing the effects of WBI on mental health, a handful of observational studies assessing the effects of WBI over time, and only short-term (up to 3-month) assessment of the effects of interventions to reduce WBI. Experimental and prospective studies are needed to better understand whether WBI causes adverse mental and physical health outcomes, or whether worse health outcomes contribute to WBI. For example, persons with depression and anxiety may be more self-critical and may anticipate negative judgments from others, which may lead to self-devaluation due to weight. Additionally, persons with more obesity-related health problems may have greater self-blame and stress, which could also contribute to WBI. A number of large-scale, prospective studies have included brief assessments of perceived weight discrimination;92, 93 inclusion of a measure of WBI in such studies, especially beginning in childhood or adolescence, could help to provide much-needed longitudinal data on the effects of WBI on health over time. As the literature on WBI becomes better established with improved measurement, more rigorous research designs, and intervention studies, meta-analyses should be prioritized to improve estimates of effect sizes and to help resolve areas of discrepancy in the literature.
A promising advancement in this research area is the recent increase in efforts to develop and test psychological interventions to reduce WBI. To date, most of these studies have been small pilot studies with short-term follow-up and, for some, without control groups. However, the large effect sizes of these interventions on reducing WBI are encouraging. Future research should continue to test interventions, on a larger scale and with long-term follow-up. In addition to assessing effects on WBI, researchers should also include both self-report and objective measures of mental and physical health. Given the reported negative associations between WBI and various indices of health, it will be important to move beyond simply documenting such associations and focus research efforts on investigating strategies for reducing WBI and, in turn, improving mental and physical health.
Acknowledgments
Funding/Conflicts of Interest: RLP is supported by a grant from NHLBI/NIH (#K23HL140176) and discloses serving as a consultant for Weight Watchers, Inc. RMP has received research funding from the Rudd Foundation and Weight Watchers, Inc.
References
- 1.Puhl RM, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 2.Puhl RM, Heuer CA. The stigma of obesity: A review and update. Obesity. 2009;17:941–64. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 3.Spahlholz J, Baer N, Konig HH, Riedel-Heller SG, Luck-Sikorski C. Obesity and discrimination - a systematic review and meta-analysis of observational studies. Obes Rev. 2016;17:43–55. doi: 10.1111/obr.12343. [DOI] [PubMed] [Google Scholar]
- 4.Schmitt MT, Branscombe NR, Postmes T, Garcia A. The consequences of perceived discrimination for psychological well-being: A meta-analytic review. Psychol Bull. 2014;140:921–48. doi: 10.1037/a0035754. [DOI] [PubMed] [Google Scholar]
- 5.Papadopoulos S, Brennan L. Correlates of weight stigma in adults with overweight and obesity: A systematic literature review. Obesity. 2015;23:1743–60. doi: 10.1002/oby.21187. [DOI] [PubMed] [Google Scholar]
- 6.Puhl RM, Suh Y. Health consequences of weight stigma: Implications for obesity prevention and treatment. Curr Obes Rep. 2015;4:182–90. doi: 10.1007/s13679-015-0153-z. [DOI] [PubMed] [Google Scholar]
- 7.Durso LE, Latner JD. Understanding self-directed stigma: Development of the Weight Bias Internalization Scale. Obesity. 2008;16:S80–S86. doi: 10.1038/oby.2008.448. [DOI] [PubMed] [Google Scholar]
- 8.Kahan S, Puhl RM. The damaging effects of weight bias internalization. Obesity. 2017;25:280–81. doi: 10.1002/oby.21772. [DOI] [PubMed] [Google Scholar]
- 9.Corrigan PW, Watson AC, Barr L. The self-stigma of mental illness: Implications for self-esteem and self-efficacy. J Soc Clin Psychol. 2006;25:875–84. [Google Scholar]
- 10.Puhl RM, Himmelstein M, Quinn D. Internalizing weight sitgma: Prevalence and sociodemographic considerations in US adults. Obesity. 2017 doi: 10.1002/oby.22029. Advance online publication. [DOI] [PubMed] [Google Scholar]
- 11.Flegal KM, Kruszon-Moran D, Carroll MD. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315:2284–91. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ogden C, Carroll M, Lawman H. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315:2292–99. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Newcomb ME, Mustanski B. Internalized homophobia and internalizing mental health problems: A meta-analytic review. Clin Psychol Rev. 2010;30:1019–29. doi: 10.1016/j.cpr.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 14.Pearl RL, Forgeard M, Rifkin L, Beard C, Bjorgvinsson T. Internalized stigma of mental illness: Changes and associations with treatment outcomes. Stigma Health. 2017;2:2–15. [Google Scholar]
- 15.Tull ES, Wickramasuriya T, Taylor J, Smith-Burns V, Brown M, Champaignie G, et al. Relationship of internalized racism to abdominal obesity and blood pressure in Afro-Caribbean women. J Nat Med Assoc. 1999;91:447–52. [PMC free article] [PubMed] [Google Scholar]
- 16.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, et al. The PRISMA Statement for reporting systematic reviews and meta-analyses for studies that evaluate health care interventions: Explanation and evaluation. PLos ONE. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sterne JAC, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, et al. ROBINS-I: A tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Heart, Lung and Blood Institute. Quality assessment tool for observational cohort and cross-sectional studies. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- 19.Carels RA, Wott CB, Young KM, Gumble A, Koball A, Oehlhof MW. Implicit, explicit and internalized weight bias and psychological maladjustment among treatment-seeking adults. Eat Behav. 2010;11:180–85. doi: 10.1016/j.eatbeh.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 20.Carels RA, Selensky JC, Rossi J, Solar C, Hlavka R. A novel stepped-care approach to weight loss: The role of self-monitoring and health literacy in treatment outcomes. Eat Behav. 2017;26:76–82. doi: 10.1016/j.eatbeh.2017.01.009. [DOI] [PubMed] [Google Scholar]
- 21.Lillis J, Thomas JG, Levin ME, Wing RR. Self-stigma and weight loss: The impact of being stigmatized. J Health Psychol. 2017 doi: 10.1177/1359105317739101. Advance online publication. [DOI] [PubMed] [Google Scholar]
- 22.Mensinger JL, Calogero RM, Tylka TL. Internalized weight stigma moderates eating behavior outcomes in women with high BMI participating in a healthy living program. Appetite. 2016;102:32–43. doi: 10.1016/j.appet.2016.01.033. [DOI] [PubMed] [Google Scholar]
- 23.Mensinger J, Meadows A. Internalized weight stigma mediates and moderates physical activity outcomes during a healthy living program for women wtih high body mass index. Psychol Sport Exerc. 2017 Advance online publication. [Google Scholar]
- 24.Berman MI, Morton SN, Hegel MT. Uncontrolled pilot study of an Acceptance and Commitment Therapy and Health at Every Size intervention for obese, depressed women: Accept Yourself! Psychotherapy. 2016;53:462–67. doi: 10.1037/pst0000083. [DOI] [PubMed] [Google Scholar]
- 25.Carels RA, Burmeister JM, Koball A, Oehlhof MW, Hinman N, LeRoy M, et al. A randomized controlled trial comparing two approaches to weight loss: Differences in weight loss maintenance. J Health Psychol. 2014;19:296–311. doi: 10.1177/1359105312470156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levin M, Potts S, Haeger J, Lillis J. Delivering acceptance and commitment therapy for weight self-stigma through guided self-help: Results from an open pilot trial. Cogn Behav Pract. 2017 Advance online publication. [Google Scholar]
- 27.Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: A preliminary test of a theoretical model. Ann Behav Med. 2009;37:58–69. doi: 10.1007/s12160-009-9083-x. [DOI] [PubMed] [Google Scholar]
- 28.Palmeira L, Cunha M, Pinto-Gouveia J. Processes of change in quality of life, weight self-stigma, body mass index, and emotional eating after an acceptance-, mindfulness-, and compassion-based group intervention (KG-Free) for women with overweight and obesity. J Health Psychol. 2017 doi: 10.1177/1359105316686668. Advance online publication. [DOI] [PubMed] [Google Scholar]
- 29.Palmeira L, Pinto-Gouveia J, Cunha M. Exploring the efficacy of an acceptance, mindfulness & compassionate-based group intervention for women struggling with their weight (Kg-Free): A randomized controlled trial. Appetite. 2017;112:107–16. doi: 10.1016/j.appet.2017.01.027. [DOI] [PubMed] [Google Scholar]
- 30.Pearl RL, Hopkins CM, Berkowitz RI, Wadden TA. Group cognitive-behavioral treatment for internalized weight stigma: A pilot study. Eat Weight Disord. 2016 doi: 10.1007/s40519-016-0336-y. Advance online publication. [DOI] [PubMed] [Google Scholar]
- 31.Essayli JH, Murakami JM, Wilson RE, Latner JD. The impact of weight labels on body image, internalized weight stigma, affect, perceived health, and intended weight loss behaviors in normal-weight and overweight college women. Am J Health Promot. 2017;31:484–90. doi: 10.1177/0890117116661982. [DOI] [PubMed] [Google Scholar]
- 32.Pearl RL, Puhl RM. The distinct effects of internalizing weight bias: An experimental study. Body Image. 2016;17:38–42. doi: 10.1016/j.bodyim.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 33.Lent MR, Napolitano MA, Wood GC, Argyropoulos G, Gerhard GS, Haves S, et al. Internalized weight bias in weight-loss surgery patients: psychosocial correlates and weight loss outcomes. Obesity Surg. 2014;24:2195–59. doi: 10.1007/s11695-014-1455-z. [DOI] [PubMed] [Google Scholar]
- 34.Meadows A, Nolan LJ, Higgs S. Self-perceived food addiction: Prevalence, predictors, and prognosis. Appetite. 2017;114:282–98. doi: 10.1016/j.appet.2017.03.051. [DOI] [PubMed] [Google Scholar]
- 35.Zuba A, Warschburger P. The role of weight teasing and weight bias internalization in psychological functioning: A prospective study among school-aged children. Eur Child Adolesc Psychiatr. 2017;26:1245–55. doi: 10.1007/s00787-017-0982-2. [DOI] [PubMed] [Google Scholar]
- 36.Vartanian LR, Pinkus RT, Smyth JM. Experiences of weight stigma in everyday life: Implications for health motivation. Stigma Health. 2016 Advance online publication. [Google Scholar]
- 37.Weineland S, Lillis J, Dahl J. Measuring experiential avoidance in a bariatric surgery population - Psychometric properties of AAQ-W. Obes Res Clin Pract. 2013;7:e464–75. doi: 10.1016/j.orcp.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 38.Palmeira L, Pinto-Gouveia J, Cunha M. The role of weight self-stigma on the quality of life of women with overweight and obesity: A multi-group comparison between binge eaters and non-binge eaters. Appetite. 2016;105:782–89. doi: 10.1016/j.appet.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 39.Webb JB, Hardin AS. An integrative affect regulation process model of internalized weight bias and intuitive eating in college women. Appetite. 2016;102:60–69. doi: 10.1016/j.appet.2016.02.024. [DOI] [PubMed] [Google Scholar]
- 40.Pearl RL, Puhl RM. Measuring internalized weight attitudes across body weight categories: Validation of the Modified Weight Bias Internalization Scale. Body Image. 2014:11. doi: 10.1016/j.bodyim.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 41.Ciupitu-Plath C, Wiegand S, Babitsch B. The Weight Bias Internalization Scale for Youth: Validation of a specific tool for assessing internalized weight bias among treatment-seeking German adolescents with overweight. J Pediatr Psychol. 2017 doi: 10.1093/jpepsy/jsx079. Advance online publication. [DOI] [PubMed] [Google Scholar]
- 42.Maiano C, Aime A, Lepage G, Team ASPQ, Morin AJS. Psychometric properties of the Weight Self-Stigma Questionnaire (WSSQ) among a sample of overweight/obese French-speaking adolescents. Eat Weight Disord. 2017 doi: 10.1007/s40519-017-0382-0. Advance online publication. [DOI] [PubMed] [Google Scholar]
- 43.Roberto CA, Sysko R, Bush J, Pearl R, Puhl RM, Schvey NA, et al. Clinical correlatees of the Weight Bias Internalization Scale in a sample of obese adolescents seeking bariatric surgery. Obesity. 2012;20:533–39. doi: 10.1038/oby.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pearl RL, Wadden TA, Hopkins CM, Shaw JA, Hayes MR, Bakizada ZM, et al. Association between weight bias internalization and metabolic syndrome among treatment-seeking individuals wtih obesity. Obesity. 2017;25:317–22. doi: 10.1002/oby.21716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barber JA, Palmese L, Reutenauer EL, Grilo CM, Tek C. Implications of weight-based stigma and self-bias on quality of life among individuals with schizophrenia. J Nerv Mental Disord. 2011;199:431–35. doi: 10.1097/NMD.0b013e318221403d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boswell RG, White MA. Gender differences in weight bias internalization and eating pathology in overweight adults. Adv Eat Dis. 2015;3:259–68. doi: 10.1080/21662630.2015.1047881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hilbert A, Braehler E, Schmidt R, Lowe B, Hauser W, Zenger M. Self-compassion as a resource in the self-stigma process of overweight and obese individuals. Obesity Facts. 2015;8:293–301. doi: 10.1159/000438681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pearl RL, White MA, Grilo CM. Weight bias internalization, depression, and self-reported health among overweight binge eating disorder patients. Obesity. 2014;22:E142–48. doi: 10.1002/oby.20617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schvey NA, White MA. The internalization of weight bias is associated with eating pathology among lean individuals. Eat Beh. 2015;17:1–5. doi: 10.1016/j.eatbeh.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 50.Schvey NA, Sbrocco T, Bakalar JL, Ress R, Barmine M, Gorlick J, et al. The experience of weight stigma among gym members with overweight and obesity. Stigma Health. 2016 Advance online publication. [Google Scholar]
- 51.Durso LE, Latner JD, White MA, Masheb RM, Blomquist KK, Morgan PT, et al. Internalized weight bias in obese patients with binge eating disorder: Associations with eating disturbances and psychological functioning. Int J Eat Disord. 2012;45:423–27. doi: 10.1002/eat.20933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hilbert A, Baldofski S, Zenger M, Lowe B, Kersting A, Braehler E. Weight Bias Internalization Scale: Psychometric properties and population norms. PLos ONE. 2014;9:e86303. doi: 10.1371/journal.pone.0086303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hain B, Langer L, Hunnemeyer K, Rudofsky G, Zech U, Wild B. Translation and validation of the German version of the Weight Self-Stigma Questionnaire (WSSQ) Obesity Surg. 2015;25:750–53. doi: 10.1007/s11695-015-1598-6. [DOI] [PubMed] [Google Scholar]
- 54.Durso LE, Latner JD, Ciao AC. Weight bias internalization in treatment-seeking overweight adults: Psychometric validation and associations wtih self-esteem, body image, and mood symptoms. Eat Behav. 2016;21:104–08. doi: 10.1016/j.eatbeh.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 55.O’Brien KS, Latner JD, Puhl RM, Vartanian LR, Giles C, Griva K, et al. The relationship between weight stigma and eating behavior is explained by weight bias internalization and psychological distress. Appetite. 2016;102:70–76. doi: 10.1016/j.appet.2016.02.032. [DOI] [PubMed] [Google Scholar]
- 56.Burmeister JM, Carels RA. Television use and binge eating in adults seeking weight loss treatment. Eat Behav. 2014;15:83–86. doi: 10.1016/j.eatbeh.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 57.Burmeister JM, Hinman N, Koball A, Hoffmann KA, Carels RA. Food addiction in adults seeking weight loss treatment. Implications for psychosocial health and weight loss. Appetite. 2013;60:103–10. doi: 10.1016/j.appet.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 58.Carels RA, Burmeister J, Oehlhof MW, Hinman N, LeRoy M, Bannon E, et al. Internalized weight bias: Ratings of the self, normal weight, and obese individuals and psychological maladjustment. J Behav Med. 2013;36:86–94. doi: 10.1007/s10865-012-9402-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Innamorati M, Imperatori C, Lamis DA, Contardi A, Castelnuovo G, Tamburello S, et al. Weight Bias Internalization Scale discriminates obesity and overweight patients with different severity levels of depression: The Italian version of the WBIS. Curr Psychol. 2017;36:242–51. [Google Scholar]
- 60.Sienko RM, Saules KK, Carr MM. Internalized weight bias mediates the relationship between depressive symptoms and disordered eating behavior among women who think they are overweight. Eat Behav. 2016;22:141–44. doi: 10.1016/j.eatbeh.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 61.Hilbert A, Braehler E, Haeuser W, Zenger M. Weight bias internalization, core self-evaluation, and health in overweight and obese persons. Obestiy. 2014;22:79–85. doi: 10.1002/oby.20561. [DOI] [PubMed] [Google Scholar]
- 62.Hubner C, Schmidt R, Selle J, Kohler H, Muller A, deZwaan M, et al. Comparing self-report measures of internalized weight stigma: The Weight Self-Stigma Questionnaire versus the Weight Bias Internalization Scale. PLos ONE. 2016;11:e0165566. doi: 10.1371/journal.pone.0165566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lillis J, Luoma JB, Levin ME, Hayes SC. Measuring weight self-stigma: The Weight Self-Stigma Questionnaire. Obesity. 2010;18:971–76. doi: 10.1038/oby.2009.353. [DOI] [PubMed] [Google Scholar]
- 64.Magallares A, Bolanos-Rios P, Ruiz-Prieto I, BenitodeValle P, Irles JA, Jauregui-Lobera I. The mediational effect of weight self-stigma in the relationship between blatant and subtle discrimination and depression and anxiety. Span J Psychol. 2017;20:1–7. doi: 10.1017/sjp.2017.1. [DOI] [PubMed] [Google Scholar]
- 65.Wang SB, Lydecker JA, Grilo CM. Rumination in patients with binge-eating disorder and obesity: Associations with eating-disorder psychopathology and weight-bias internalization. Eur Eat Disord Rev. 2017;25:98–103. doi: 10.1002/erv.2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schvey NA, Roberto CA, White MA. Clinical correlates of the Weight Bias Internalization Scale in overweight adults with binge and purge behaviours. Adv Eat Disord. 2013:1. [Google Scholar]
- 67.Sevincer GM, Kaya K, Bozkurt S, Akin E, Kose S. Reliability, validity, and factorial structure of the Turkish version of the Weight Self-Stigma Questionnaire (Turkish WSSQ) Psychiatr Clin Psychopharmacol. 2017;27:386–92. [Google Scholar]
- 68.Almenara CA, Aime A, Maiano C, Ejova A, Guevremont G, Bournival C, et al. Weight stigmatization and disrodered eating in obese women: The mediating effects of self-esteem and fear of negative appearance evaluation. Eur Rev Appl Psychol. 2017;67:155–62. [Google Scholar]
- 69.Pearl RL, White MA, Grilo CM. Overvaluation of shape and weight as a mediator between self-esteem and weight bias internalization among patients with binge eating disorder. Eat Behav. 2014;15:259–61. doi: 10.1016/j.eatbeh.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Palmeira L, Pinto-Gouveia J, Cunha M, Carvalho S. Finding the link between internalized weight-stigma and binge eating behaviors in Portugese adults women with overweight and obesity: The mediator role of self-criticism and self-reassurance. Eat Behav. 2017;26:50–54. doi: 10.1016/j.eatbeh.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 71.Jung F, Spahlholz J, Hilbert A, Riedel-Heller S, Luck-Sikorski C. Impact of weight-related discrimination, body dissatisfaction, and self-stigma on the desire to weigh less. Obesity Facts. 2017;10:139–51. doi: 10.1159/000468154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lin KP, Lee ML. Validating a Chinese version of the Weight Self-Stigma Questionnaire for use with obese adults. Int J Nurs Pract. 2017;23:e12537. doi: 10.1111/ijn.12537. [DOI] [PubMed] [Google Scholar]
- 73.Durso LE, Latner JD, Hayashi K. Perceived Discrimination is Associated with Binge Eating in a Community Sample of Non-Overweight, Overweight, and Obese Adults. Obesity Facts. 2012;5:869–80. doi: 10.1159/000345931. [DOI] [PubMed] [Google Scholar]
- 74.Pearl RL, Dovidio JF. Experiencing weight bias in an unjust world: Impact on exercise and internalization. Health Psychol. 2015;34:741–49. doi: 10.1037/hea0000178. [DOI] [PubMed] [Google Scholar]
- 75.Douglas V, Varnado-Sullivan P. Weight stigmatization, internalization, and eating disorder symptoms: The role of emotion dysregulation. Stigma Health. 2016;1:166–75. [Google Scholar]
- 76.Baldofski S, Rudolph A, Tigges W, Herbig B, Jurowich C, Kaiser S, et al. Weight bias internalization, emotion dysregulation, and non-normative eating behaviors in prebariatric patients. Int J Eat Disord. 2016;49:180–85. doi: 10.1002/eat.22484. [DOI] [PubMed] [Google Scholar]
- 77.Raves DM, Brewis A, Trainer S, Han S, Wutich A. Bariatric surgery patients’ perceptions of weight-related stigma in healthcare settings impair post-surgery dietary adherence. Front Psychol. 2016;7:1497. doi: 10.3389/fpsyg.2016.01497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Himmelstein MS, Puhl RM, Quinn DM. Intersectionality: An understudied framework for addressive weight stigma. Am J Prev Med. 2017;53:421–31. doi: 10.1016/j.amepre.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 79.Puhl RM, Quinn D, Weisz B, Suh Y. The role of stigma in weight loss maintenance among U.S. adults. Ann Behav Med. 2017 doi: 10.1007/s12160-017-9898-9. [DOI] [PubMed] [Google Scholar]
- 80.Farhangi MA, Emam-Alizadeh M, Hamedi F, Jahangiry L. Weight self-stigma and its association with quality of life and psychological distress among overweight and obese women. Eat Weight Disord. 2017;22:451–56. doi: 10.1007/s40519-016-0288-2. [DOI] [PubMed] [Google Scholar]
- 81.Latner JD, Durso LE, Mond JM. Health and health-related quality of life among treatment-seeking overweight and obese adults: associations with internalized weight bias. J Eat Disord. 2013:1. doi: 10.1186/2050-2974-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Latner JD, Barile JP, Durso LE, O’Brien KS. Weight and health-related quality of life: The moderating role of weight discrimination and internalized weight bias. Eat Behav. 2014;15:586–90. doi: 10.1016/j.eatbeh.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 83.Lillis J, Levin ME, Hayes SC. The relationship between body mass index and health-related quality of life: A pilot study of the impact of weight self-stigma and experiential avoidance. J Health Psychol. 2011;16:722–27. doi: 10.1177/1359105310388321. [DOI] [PubMed] [Google Scholar]
- 84.Pearl RL, Puhl RM, Dovidio JF. Differential effects of weight bias experiences and internalization on exercise among women with overweight and obesity. J Health Psychol. 2015;20:1626–32. doi: 10.1177/1359105313520338. [DOI] [PubMed] [Google Scholar]
- 85.Puia IC, Stanculete MF, Hopulele-Petri A, Muresan D, Puia A. Patients’ perception of weight-related stigma in a Romanian sample. J Evid Based Psychother. 2017;17:147–57. [Google Scholar]
- 86.Koball AM, Mueller PS, Craner J, Clark MM, Nanda S, Kebede EB, et al. Crucial conversations about weight management wtih healthcare providers: Patients’ perspectives and experiences. Eat Weight Disord. 2016 doi: 10.1007/s40519-016-0304-6. Advance online publication. [DOI] [PubMed] [Google Scholar]
- 87.Lee MS, Dedrick RF. Weight Bias Internalization Scale: Psychometric properties using alternative weight status classification. Body Image. 2016;17:25–29. doi: 10.1016/j.bodyim.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 88.Hubner C, Baldofski S, Zenger M, Tigges W, Herbig B, Jurowich C, et al. Influences of general self-efficacy and weight bias internalization on physical activity in bariatric surgery candidates. Surg Obes Relat Disord. 2015;11:1371–76. doi: 10.1016/j.soard.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 89.Eisenberg MH, Street RL, Persky S. “It runs in my family…”: The association of perceived family history with body dissatisfaction and weight bias internalization among overweight women. Women Health. 2017;57:478–93. doi: 10.1080/03630242.2016.1170095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Becker CB, Middlemass K, Taylor B, Johnson C, Gomez F. Food insecurity and eating disorder pathology. Int J Eat Disord. 2017;50:1031–40. doi: 10.1002/eat.22735. [DOI] [PubMed] [Google Scholar]
- 91.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: A test of the HIV Stigma Framework. AIDS Behav. 2013;17:1785–95. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sutin AR, Stephan Y, Terracciano A. Weight discrimination and mortality. Psychol Sci. 2015;26:1803–1811. doi: 10.1177/0956797615601103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jackson SE, Beeken RJ, Wardle J. Perceived weight discrimination and changes in weight, waist circumferance, and weight status. Obesity. 2014;22:2485–88. doi: 10.1002/oby.20891. [DOI] [PMC free article] [PubMed] [Google Scholar]